Introduction
Aging is a multi-factorial process
defined as time-dependent general decline in physiological function, which is
associated with a progressively increasing risk of frailty, morbidity and
mortality [1,2]. The
effect of aging is mainly observed in modern human societies and in animals
under laboratory conditions [3]. The
dramatic increase in mean human life span and life expectancy, coupled to a
significant reduction in early mortality caused by the reduced occurrence of
infections during the past two centuries, has led to an enormous increase in
the number of elderly people in modern societies [4,5]. This
demographic phenomenon has been paralleled by an epidemic of chronic diseases
associated with advanced age, most of which have complex etiology and
underlying pathogenic mechanisms [6]. Intensive
efforts have been made over the last decades to identify single key players involved in
age-related diseases. Poly(ADP-ribose) polymerase 1 (PARP1) is a chromatin-associated
nuclear protein which functions as stress sensor and as such is involved in the
cellular responses to a variety of age-related stress signals.
Poly(ADP-ribose)
polymerase 1 as molecular stress sensor
PARP1 is an abundant nuclear chromatin-associated
multifunctional enzyme found in most eukaryotes apart from yeast [7]. PARP1 has
been initially thought to be the only existing enzyme with
poly(ADP-ribosyl)ation activity in mammalian cells. However, five additional Parp-like
genes encoding "bona fide" PARP enzymes have been identified in recent
years, indicating that PARP1 belongs to a family of "bona fide" PARP enzymes [8]. The basal enzymatic activity of PARP1 is very
low, but is stimulated dramatically under conditions of cellular stress [9,10]. Activation of PARP1 results in
the synthesis of poly(ADP-ribose) (PAR) from nicotinamide adenine dinucleotide
(NAD+) and in the release of nicotinamide as reaction by-product [7,8]. Following PARP1 activation,
intracellular PAR levels can rise 10-500-fold [11-13]. Despite intensive research on the cellular
functions of PARP1, the molecular mechanism of PAR formation has not been
comprehensively understood. Up to now, two different modes of PARP1 activation have been described,
one dependent on DNA damage and one dependent on post-translational protein
modifications (see below).
PAR
is a heterogeneous linear or branched homo-polymer of repeating ADP-ribose units
linked by glycosidic ribose-ribose bonds [7,9,14]. Most free or
protein-associated PAR molecules are rapidly degraded in vivo [15]. This rapid
turnover strongly suggests that PAR levels are tightly regulated under
physiological stress conditions and that degradation of the polymer starts
immediately upon initiation of PAR synthesis. To date two enzymes,
poly(ADP-ribose) glycohydrolase (PARG) and ADP-ribosyl protein lyase, have been
described to be involved in PAR catabolism [16,17]. While PARG
possesses both exo- and endoglycosidic activities, the lyase has been described
to cleave
the bond between proteins and mono(ADP-ribose). The attachment of negatively charged
PAR onto proteins is transient but can be very extensive in vivo, as
polymer chains can reach more than 400 units on protein acceptors [7]. PAR formation
has been implicated in a variety of cellular processes, such as maintenance of
genomic stability, transcriptional regulation, energy metabolism and cell death
[7]. The
physiological consequences of this post-translational modification on the
molecular level, however, are not yet completely understood. It has been
proposed that PAR may have a dual role in modulating cell survival and cell
death [9,18,19]. Low to
moderate levels of PAR may be beneficial for important cellular functions,
whereas extensive PAR formation can be detrimental and lead to various forms of
cell death. More than a decade ago, PARP1 activity was linked to the aging
process, as poly(ADP-ribosyl)ation capacity was shown to correlate with
species-specific longevity [20,21].
Most
proteins associated with PAR are nuclear DNA-binding proteins, including PARP
family members and histones [7,22,23]. PARP1 is the
main acceptor for poly(ADP-ribosyl)ation in vivo and auto-modification
of PARP1 abolishes its affinity for NAD+ and DNA [24,25]. A similar
effect has been postulated for histones/nucleosomes. PAR polymers could
function to alter chromatin conformation through covalent or non-covalent
interactions with histone tails and via displacement of histones from DNA, thus
regulating the accessibility of the genetic material. It was suggested that PAR
might either directly participate in chromatin remodelling processes or
indirectly coordinate them through recruitment and regulation of specific
chromatin remodelling proteins [7,22]. Moreover, PAR
is recognized and bound by macrodomain containing histone variants [26].
Over
20 years ago, Nathan Berger was the first to suggest that cellular stress (e.g.
oxidative damage) causes over-activation of PARP1 and subsequent NAD+
depletion [27,28]. In an attempt
to restore the NAD+ pools, NAD+ is resynthesized with a
consumption of 2-4 molecules of ATP per molecule of NAD+. As a
consequence, cellular ATP levels become depleted, leading to subsequent energy
failure, which results in cellular dysfunction and eventually in necrotic cell
death [27,28].
Pharmacological inhibition
of the enzymatic activity of PARP or the complete absence of PARP1 was shown to
significantly improve cellular energetic status and cell viability after
exposure to necrosis-inducing agents [29-31]. The
contribution of poly(ADP-ribosyl)ation reactions to necrotic cell death seems
to be dependent on the cell type and the cellular metabolic status [7,32,33].
Interestingly,
genetic studies using Parp1 knockout mice provided preliminary evidence
that energy depletion alone might not be sufficient to mediate
poly(ADP-ribosyl)ation-dependent cell death [34]. A second model
has been proposed to explain how PARP1 regulates cell death. This model
suggests that over-activation of PARP1 induces translocation of
apoptosis-inducing factor (AIF) from the mitochondria to the nucleus, causing
DNA condensation and fragmentation, and subsequent cell death [35].
Together,
PARP1 can be regarded as molecular stress sensor with many physiological
cellular functions. Over-activation of PARP1 results in the generation of large
amounts of PAR. Subsequently, cellular NAD+ pools are depleted and
AIF is released from the mitochondria to trigger cell death. Importantly, these
PARP1-dependent cellular suicide mechanisms have been implicated in the
pathomechanisms of neuro-degenerative disorders, cardiovascular dysfunction and
various other forms of inflammation [36].
Activation of PARP1 by
reactive oxygen species (ROS)
A
unified theory explaining the pathogenesis of diverse degenerative conditions
in different organs (including Alzheimer's, Parkinson's and other
neurodegenerative disorders, rheumatoid arthritis, atherosclerosis and other
cardiovascular diseases, diabetes) has been proposed to explain how the single
physiological process of aging may lead to diverse pathological states [37]. This
oxidative stress theory of aging (or free radical theory of aging), initially
proposed by Harman in 1956, provides the most plausible and currently
acceptable global mechanism to explain the aging process [38]. The theory
postulates that aging is, in the absence of other risk factors (e.g.
infections, smoking, hypercholesterolemia), the net consequence of free
radical-induced damage and the inability to counter-balance these changes by
anti-oxidative defenses. An increase in intracellular ROS levels through
hydrogen peroxide treatment of cells or through the inhibition of ROS scavenging
enzymes, such as superoxide dismutase (SOD1), causes premature senescence and
can shorten cellular life span [39-45].
Mitochondria are the main producers of cellular ROS under normal conditions, as
approximately 1-2% of the oxygen molecules consumed during respiration are
converted into highly reactive superoxide anions [46]. Besides
aerobic metabolism in mitochondria, β-oxidation in
peroxisomes and certain enzymes can produce ROS. Intracellular ROS can damage
cellular components through oxidation of macromolecules such as nucleic acids,
proteins and lipids [47]. Moreover,
an overproduction of ROS leads to rapid generation of peroxinitrite from nitric
oxide and superoxide, causing an imbalance in nitric oxide signaling [48].
Since the oxidative stress theory was
first proposed, a considerable body of evidence has been published
corroborating the idea that increased production of ROS underlies cellular
dysfunction in various organ systems of aged humans and laboratory animals [49].
Interestingly, the enzymatic activity of PARP1 can be strongly activated by
treatment of cells with ROS such as hydrogen peroxide [8]. Earlier
studies described that PARP1 binds to oxidative damage-induced strand breaks
within the DNA via two zinc finger motifs and thereby becomes activated [9]. More
recently, several studies suggested that PARP1 activity is also regulated in a
DNA-independent manner. A proteomic investigation uncovered many
ERK1/2-induced phosphorylation sites in PARP1, which are located within
important functional domains, consistent with regulatory roles in vivo [50,51].
Furthermore, DNA-independent PARP1 activation can be triggered by the direct
interaction of PARP1 with phosphorylated ERK-2 without PARP1 being
phosphorylated itself [52]. In
addition, PARP1 can be activated by elevated levels of extracellular glucose,
Ca2+ and angiotensin II, and allosteric regulation of
auto-poly(ADP-ribosyl)ation by Mg2+, Ca2+, polyamines,
ATP and the histones H1 and H3 has been reported [53]. Whether
ROS-mediated activation of PARP1 is due to ROS-generated DNA damage or also
based on other ROS-induced cellular (signaling) mechanisms awaits further
investigations.
PARP1 is linked to energy metabolism through NAD+
NAD+ biosynthesis has become of
considerable interest due to the important signaling functions of pyridine
nucleotides. In mammals, niacin (collectively designating nicotinamide and
nicotinic acid) and the essential amino acid tryptophan are precursors of NAD+ biosynthesis
[12,54]. The formation of dinucleotides from ATP and the mononucleotide of
niacin constitute the most critical step in NAD+generation, which is catalyzed by
NMN/NaMN adenylyltransferases (NMNATs) [13,55]. Since PARP1 uses NAD+ as substrate to
synthesize PAR, PARP1 decisively depends on the amount of NAD+
available and may act as energy sensor in the nucleus. Both constitutive and
activated levels of PAR have been suggested to be strictly dependent on the
concentration of NAD+ in cells [15,56,57]. Importantly, the nuclear concentration of NAD+ can
be modulated by NMNAT-1 and a recent study revealed that NMNAT-1 is able to
interact with and stimulate PARP1 [58]. It is thus
tempting to speculate that PARP1 activation is supported by the localized
action of NMNAT-1. Depending on the level of PARP1 activity, the cellular NAD+
concentration is concomitantly reduced. Therefore, PARP1 not only is a sensor
of NAD+, but in turn also influences cellular energy levels.
Dietary
restriction, also called calorie restriction, is defined as a life-long
moderate (20-40%) reduction in caloric intake and has repeatedly been shown to
extend the longevity of both invertebrates and vertebrates [59,60].
Reducing the caloric intake starting even at an old age has also been shown to
increase the life span of flies and mice and is sufficient to reverse gene
expression changes associated with aging [61-63].
Furthermore, dietary restriction in rodents delays the onset and reduces the
severity of many age-related diseases, such as cardiovascular disease,
diabetes, osteoporosis, cataracts, neurodegenerative disease and cancers [60]. Although
it was initially expected that dietary restriction would reduce overall
cellular energy levels byslowing down
glycolysis and the tricarboxylic acid (TCA) cycle [59], this
assumption has been challenged, since
dietary restriction was shown to cause an increase in NAD+/NADH
ratios in yeast cultures [64]. Whether
this is also the case in mammalian cells remains to be determined. Along the
same lines, the impact of dietary restriction on enzymes that depend on NAD+
(e.g. PARP1) is currently being investigated in multiple laboratories. Whether
and how PARP1 activation differs in species with different maximal life span
(and possibly also with different cellular NAD+ pools), however,
remains an open question.
Crosstalk
between PARP1 and other NAD+-consuming enzymes
NAD+ is an essential cofactor regulating numerous cellular
pathways and has recently been recognized as a substrate for a growing number
of NAD+-dependent enzymes [11,13].
NAD+-dependent post-translational protein modifications
are catalyzed by several enzyme families, including PARPs and the sirtuin
family of NAD+-dependent class III histone deacetylases (SIRTs) [8,65,66].
SIRTs and the yeast homolog and founding member of the sirtuins, Sir2, are
induced by dietary restriction and have been implicated in senescence and
aging, although the exact mechanisms are not yet known [59,67]. Intriguingly, ADP-ribosylation by PARP1 could modulate
the NAD+-dependent deacetylation of proteins by SIRTs via the NAD+/nicotinamide
connection. The decline of NAD+ levels and the rise of nicotinamide
upon PARP1 activation have immediate effects on other NAD+-consuming
enzymes [57,68,69]. SIRTs require NAD+ as substrate and are
inhibited by low levels of nicotinamide [70].
Consequently, under conditions of cellular stress and PARP1 activation, the
activity of SIRTs is downregulated.
PARPs and sirtuins may not only compete
for the same substrate, but might also regulate each other more directly. For
instance, PARP1 and SIRT1 interact at the protein level and SIRT1 might be
regulated by PARP1-dependent trans-ADP-ribosylation [7]. Another
link between PAR generation and acetylation/deacetylation reactions comes from
the very recent identification of three lysine residues in the
auto-modification domain of PARP1 as acceptor sites for auto-ADP-ribosylation [71]. The same lysines
were previously identified as targets for acetylation by p300 and PCAF [72]. Remarkably,
simple addition of PCAF reduced poly(ADP-ribosyl)ation of PARP1 (own
unpublished observation), suggesting that the interaction domain of PARP1 with
PCAF is overlapping with the ADP-ribose acceptor sites. We recently also
published that acetylation of lysine residues interferes with ADP-ribosylation [73]. This
finding points at an interesting crosstalk between acetylation of and
ADP-ribosylation by PARP family members. It will certainly be interesting to
further investigate the crosstalk between PARP1-dependent
ADP-ribosylation and acetylation/ deacetylation
reactions. NAD+ levels can be expected to play an important role for
the interplay between these two NAD+-dependent post-translational
protein modifications. Whether the balance between and the tight regulation of
poly(ADP-ribosyl)ation and NAD+-dependent deacetylation is altered
during aging remains to be investigated. Furthermore,
it will be important to identify additional NAD+-dependent enzymes
involved in the aging process.
Emerging pathological evidence indicates that major
chronic age-related diseases, such as atherosclerosis, arthritis, dementia,
osteoporosis and cardiovascular disease, are inflammation-related [74]. A link between NAD+ metabolism and the regulation of an inflammatory
response is suggested by the finding that nicotinamide phosphoribosyltransferase
(NAMPT), one of the enzymes involved in NAD+ biosynthesis from nicotinamide, increases cellular
NAD+ levels in response to stress [75]. The
expression of NAMPT is upregulated in activated lymphocytes [76].
Furthermore, NAMPT protein
and/or mRNA levels were also found to be upregulated upon stimulation of immune
cells both in vivo and in vitro [77,78], whereas a specific NAMPT inhibitor was found to inhibit cytokine
production [79]. Notably, nicotinamide is known to inhibit
the production of key inflammatory mediators [80-82], protects neurons against excitotoxicity [83,84], and blocks replicative senescence of primary cells [85]. Moreover, a
recent study suggested that intracellular NAD+ levels regulate TNF-α protein synthesis in a SIRT6-dependent
manner [86]. Both, SIRT1 and SIRT6 also regulate NF-κB signaling with effects on senescence and possibly aging [87,88].
Together, accumulating evidence suggests that cellular
NAD+ biosynthesis and the NAD+-consuming reactions
poly(ADP-ribosyl)ation and SIRT-dependent deacetylation are tightly
interrelated and have functions in inflammation and age-related diseases.
PARP1 is linked to age-related inflammation as
transcriptional cofactor of NF-κB
A body of experimental and clinical evidence suggests
that the immune system is implicated in almost all age-related or associated
diseases [89,90]. There
is a well-established connection between oxidative stress and the inflammatory
immune response [37]. A
prominent mechanism by which age-induced ROS modulate inflammation is by
inducing the redox-sensitive transcription factor nuclear factor kappa B (NF-κB). This induction of NF-κB leads to the
generation of pro-inflammatory mediators and a state of chronic inflammation [91,92]. NF-κB plays an important role in inflammatory phenotypic changes in various
pathophysiological conditions [49]. In fact,
NF-κB has a fundamental role in mediating all the
classical attributes of inflammation - rubor, calor, dolor and tumor - by
regulating transcriptional programs in tissues containing epithelial and
stromal cells, vascular endothelial cells and hematopoietic cells [93]. During the
last decade, it has been clearly demonstrated that excessive activation or
inappropriate regulation of immune and inflammation cascades causes tissue and
cellular damage, which can lead to cellular dysfunction and death [14].
Furthermore, it was suggested that chronic, low-grade inflammation is a
possible converging process linking normal aging and the pathogenesis of
age-related diseases [94]. This
hypothesis is in accordance with the finding that constitutive activation of
NF-κB, accompanied by elevated levels of inflammatory markers,
is a ubiquitous phenomenon observed in various cell types in the aging
phenotype [95].
In most unstimulated cells, NF-κB is sequestered in the cytoplasm as an inactive transcription factor
complex by its physical association with one of several inhibitors of NF-κB (IκB) [96-100]. The
key regulatory event in NF-κB induction is the
phosphorylation of IκB proteins by the IκB kinase (IKK)
complex, which leads to IκB protein ubiquitylation and subsequent degradation [101,102]. ROS have been reported to induce the
activation of NIK/IKK and MAPK pathways that lead to the degradation of IκB and subsequent NF-κB-dependent gene expression [74,103]. Conversely,
induction of NF-κB itself results in the generation of ROS via the
expression of inducible nitric oxide synthase (iNOS), thus activating a
feedback loop that amplifies the process of damage and deterioration in target
cells and organs [37].
Global screens for age-specific gene
regulation have been performed from many tissues in mice and humans [3]. These
analyses have recently provided evidence that the NF-κB binding domain is the genetic regulatory motif most strongly
associated with the aging process and thatNF-κB target genes show a strong increase in expression with age in human
and mouse tissues as well as in stem cells [104-106].
Furthermore, NF-κB is implicated in age-dependent induction of cellular
senescence in epithelial and hematopoietic progenitor cells [104,107].
Blockade of NF-κB in the skin of aged mice can reverse the global gene
expression program and tissue characteristics to that of younger animals [108]. Moreover,
Donato et al. reported lately that in vascular endothelial cells of aged human
donors nuclear NF-κB levels increase, IκBα levels decrease and that the expression of proinflammatory cytokines,
such as interleukin 6 (IL-6), tumor
necrosis factor-α (TNF-α) and monocyte chemoattractant protein 1 (MCP-1) is reduced [109]. NF-κB activity was also increased in aged rat vessels and kidneys, but
reduced in rats under calorie restriction [110,111].
Studies
performed with Parp1 knockout mice have identified various detrimental
functions of PARP1 in inflammatory and neurodegenerative disorders. Parp1
gene-disruption protected from tissue injury in various oxidative
stress-related disease models ranging from stroke, (MPTP)-induced parkinsonism,
myocardial infarction, streptozotocin-induced diabetes, lipopolysaccharide-induced
septic shock, arthritis, to colitis and zymosan-induced multiple organ failure [7,73,112,113].
There are striking similarities between the expression pattern of PARP1 and the
detrimental transcriptional activity of NF-κB. In most tissues
and cell types associated with high PARP1 expression, dysregulated NF-κB activity seems to contribute to cellular dysfunction and necrotic
cell death during inflammatory disorders [14]. The
strongest indication for a direct role of PARP1 in NF-κB-dependent transcription was the impaired expression of NF-κB-dependent pro-inflammatory mediators in Parp1 knockout mice [113]. Moreover,
the upregulation of several inflammatory response genes after treatment with
inflammatory stimuli was drastically reduced in Parp1 knockout mice [112,114-116].
Our group provided first evidence that PARP1 is required for specific NF-κB-dependent gene activation and can act as transcriptional coactivator
of NF-κB in vivo [117]. PARP1 is
required and sufficient for specific transcriptional activation of NF-κB in response to pro-inflammatory stimuli and cellular stress.
Furthermore, Tulin and Spradling found that Drosophila mutants lacking normal
PARP levels display immune defects similar to mice lacking the NF-κB subunit p50 [118].
These results imply that the role of PARP1 in NF-κB-dependent gene
expression during immune responses has been conserved during evolution.
Together, several lines of evidence suggest a model in which PARP1 functions as
a promoter-specific cofactor for NF-κB-dependent gene
expression [7,14].
PARP
as therapeutic target for age-associated diseases
During
the last two decades of intensive research, over 50 potential PARP inhibitors
were developed [119]. The
involvement of PARP1 in cell death (both apoptosis and necrosis) and the
capacity of PARP1 to promote the transcription of pro-inflammatory genes are
particularly important for drug development. On the basis of structural
information available for the catalytic domains of PARP1 and PARP2
co-crystallized with NAD+ or certain PARP inhibitors, it became
clear that the majority of PARP inhibitors mimic the nicotinamide moiety of NAD+and bind to the donor site within the catalytic domain [120-122]. Although the physiological
functions of PARPs and poly(ADP-ribosyl)ation is still under debate, numerous experimental studies during the last years
have clearly demonstrated the beneficial effects of PARP inhibition from cell
culture systems to pre-clinical animal models of acute and chronic inflammation [36,119]. For
instance, Vaziri and colleagues observed an extension of cellular life span
when PARP activity was inhibited [123]. In animal
studies, PARP inhibition and/or PARP1 deficiency is effective in different
age-related diseases [119]. The PARP inhibitor 5-AIQ has been demonstrated to
attenuate the expression of P-selectin and intracellular adhesion molecule-1
(ICAM-1) as well as the recruitment of neutrophils and leukocytes into the
injured lung [124,125].
Thus, application of inhibitors reduces the degree of acute inflammation and
tissue damage associated with experimental lung injury. As ROS released from
the recruited leukocytes cause an upregulation of adhesion molecules, treatment
with PARP inhibitors contributes to the termination of this vicious cycle and
inhibits the inflammatory process. Similar to the effects of pharmacological
inhibitors, Parp1 knockout mice were found to be resistant against
zymosan-induced inflammation and multiple organ failure when compared with the
response of wild-type animals [126].
In murine models of arthritis, inhibition of PARP with
nicotinamide delayed the onset of the disease and reduced the progress of established
collagen-induced arthritis [127].
5-iodo-6-amino-1,2-benzopyrone and PJ34, two novel PARP inhibitors, were
beneficial in a mouse model of collagen-induced arthritis by reducing both the
incidence of arthritis and the severity of the disease [128,129].
Similarly, GPI 6150 was found to be highly effective in a rodent model of
adjuvant-induced arthritis [130].
PARP activation also has a pathogenic
role in hypertension, atherosclerosis and diabetic cardiovascular complications
[119,131]. In these diseases, the function of the vascular endothelium is
impaired, resulting in a reduced ability of the endothelial cells to produce
nitric oxide and other cytoprotective mediators. This then sets the stage for
many manifestations of cardiovascular disease. The oxidant-mediated endothelial
cell injury is dependent on PARP1 and can be attenuated by pharmacological
inhibitors or genetic PARP1 deficiency [115,132].
Furthermore, PARP inhibition improves aging-associated cardiac and endothelial
dysfunction [133].
In general, the severity of many inflammatory diseases
is suppressed by PARP inhibitors and the production of multiple
pro-inflammatory mediators is downregulated [48]. The
inhibition of PARP also reduces the formation of nitrotyrosine in inflamed
tissues, an indicator of reactive nitrogen species. This finding was, at first,
unexpected because PARP activation is perceived to occur downstream of the
generation of oxidants and free radicals in various diseases. The mechanism is
probably related to the fact that PARP inhibition reduces the infiltration of
neutrophils into inflammatory sites [126]. This in
turn reduces oxygen- and nitrogen-centered free-radical production. The basis
for the regulation of neutrophil infiltration by PARP might be related to the
reduced expression of adhesion molecules [134,135]
and/or the preservation of endothelial integrity [115,132].
Alternatively, the reduction of nitrotyrosine could be explained by the finding
that PARP1 is required for the expression of iNOS, the main producer of nitric
oxide in inflamed tissues [116]. In
summary, multiple studies suggest that a tight regulation of PARP activity is
required to prevent a variety of age-related pathological conditions.
Role of PARP1's enzymatic activity in NF-κB -dependent gene expression
There is no consensus in the literature as to whether
the modulation of NF-κB-mediated transcription by PARP1 is dependent on
poly(ADP-ribosyl)ation or, alternatively, merely on the physical presence of
PARP1 [14]. Genetic
approaches provide strong evidence that poly(ADP-ribosyl)ation is not affecting
the DNA binding activity of NF-κB and is not required for NF-κB-dependent gene expression [14,136].
Neither the enzymatic activity of PARP1 nor its binding to DNA was required for full
activation of NF-κB in response to various stimuli in vivo when
tested on transiently transfected reporter plasmids [137,138].
Consistently, the enzymatic activity of PARP1 was not required for full
transcriptional activation of NF-κB in the presence of
the histone acetyltransferase p300 [72]. At first
glance this seems not to be compatible with reports describing that PARP inhibitors abolish mRNA expression of iNOS,
IL-6 and TNF-α in cultured cells [139] or that PARP inhibitors reduce the expression of inflammatory
mediators in mice [124,126,140].
However, this discrepancy might be explained in three ways: First, it should be noted that the currently available PARP
inhibitors do not discriminate well between PARP1 and other PARP family members
or even other NAD+-metabolizing enzymes, which are described to also play a role in inflammatory response
pathways [139,141]. In Parp1 knockout mice, PAR formation is indeed drastically
reduced only in brain, pancreas, liver, small intestine, colon, and testis,
whereas still moderate levels of residual poly(ADP-ribose) formation can
be observed in the stomach, bladder, thymus, heart, lung, kidney and spleen [7]. This
residual activity can most likely be attributed to PARP2, which has the
greatest similarity to PARP1 among all PARP family members [8].
Interestingly, PARP2 is involved in T lymphocyte development and survival [142] and has
been implicated in inflammatory immune responses [143,144].
A putative role of PARP2 in aging awaits further investigations. Second,
based on recent reports, one cannot exclude the possibility
that PARP-inhibitors might even affect non-NAD+-consuming targets
such as AKT/PKB or MMPs [145]. Third,
the enzymatic activity of PARP1 might be required for the transcriptional
activity of transcription factors involved in inflammatory processes other than
NF-κB. Several groups have shown that co-operative
activities between transcription factors such as AP-1, STAT-1 or IRF-1 in the
enhanceosomes of NF-κB dependent genes are required for full synergistic
activation of target genes [146,147]. Considering
these constraints of all currently available PARP
inhibitors, the specific contribution of PARP1 enzymatic activity for
age-related diseases, in which PARP inhibition has beneficial effects, needs to
be evaluated very carefully.
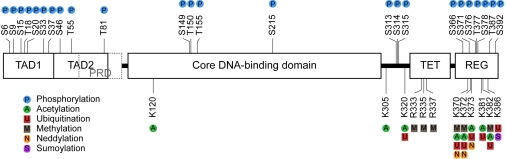
Figure 1. PARP1 at the crossroad of metabolic stress and inflammation in aging. PARP1 is
activated by cellular stress, e.g. by oxidative damage due to increased
levels of reactive oxygen species (ROS). As NAD+-dependent
enzyme, PARP1 senses energy levels and crosstalks with other NAD+-consuming
enzymes. Over-activation of PARP1 leads to energy depletion and cell death.
On the other hand, PARP1 functions as cofactor for NF-κB-dependent transcription and is
therefore implicated in many inflammatory processes. Both, PARP1-mediated
metabolic stress and PARP1-regulated inflammation can lead to tissue
degeneration underlying many age-related pathologies. See text for further
details.
The authors acknowledge the contributions by
researchers whose work could not be cited in this review due to space
limitations. We thank Paul O. Hassa and Ingrid Kassner (both Institute of
Veterinary Biochemistry and Molecular Biology, University of Zurich, Zurich,
Switzerland) for critical reading of the manuscript and helpful discussions.
Our own research on PARP1 is supported by SNF grants 31-109315.05 and 31-122421.08.
The authors in this manuscript have no conflict of
interests to declare.