In this study, we summarized the clinical characteristics and treatment outcome of 236 COVID-19 patients who were diagnosed before February 14 in Changsha city. About 20% patients were severe and critical type. Two patients died due to the severe disease. The 10-, 14-, 20- and 28-day discharge rate was 19.1%, 42.8%, 65.0% and 76.4%, respectively. The 10-, 14-, 20- and 28-day discharge rate for mild / general patients and severe / critical patients were 21.6%, 45.8%, 67.1%, 75.0% and 8.7%, 30.4%, 56.1%, 77.6%, respectively.
Compared to patients with mild or general type, discharged patients who presented with severe or critical type had longer median length of hospital stay (LOH) (12 [IQR, 10-16] days vs 15 [IQR, 12-20]; P=0.006). In addition, severe / critical patients were older, more likely to visit Wuhan, get in touch with Wuhan people. Mild / general patients were more likely to be infected by patients and family members. Severe/critical patients were more likely to have comorbidities, such as hypertension, heart disease and chronic kidney disease. Severe/critical patients were more likely to have symptoms, such as fever, fatigue, dyspnea, etc. Moreover, severe / critical patients had lower lymphocyte and platelet counts. TCM Xuebijing were used more frequently in severe / critical patients and this drug showed significant benefit in severe / critical patients.
The coronavirus disease-19 (COVID-19) spreads rapidly and has obvious family aggregation [7]. Currently, there are no specific antiviral drugs to kill the virus (treatment guideline). Comprehensive management and active symptomatic treatment are the main treatment strategies. As COVID-19 is a respiratory infectious disease with strong transmission, we need high personal protection requirements for doctors and nurses. Comprehensive strategies have played important roles in decreasing the mortality rate and preventing the infection of medical workers. Here, we summarized three main strategies, including the treatment strategy, infection control strategy, and safeguard strategy.
The first one is the treatment strategy
1.1 For mild patients, doctor in charge assessed patient’s condition daily according to the patient’s symptoms, vital signs and oxygen saturation. Patients who had no fever at 3-5 days after hospitalization received coronavirus nucleic acid tests and CT scan for doctors to detect disease changes. As shown in Table 1, 160 (67.2%) cases reported having fever before hospitalization, but the majority of patients had no fever after admission. As shown in Table 2, only 58 (24.3%) patient had fever and most of them (42 [72.4%]) were low-fever (37.3-38.0 °C).
Among 94 patients who had no fever after admission, 16 patients were found obvious glass-like changes in bilateral lungs by CT scan at three days later post-admission. That was a sign for disease exacerbation from mild to severe. At that moment, the addition of pure oxygen inhalation, low-dose glucocorticoid and short-term gamma-globulin therapy was necessary. By above treatment, 15 patients turned back to mild, 10 of whom turned to mild in 2-6 days; the rest 5 patients turned to mild in 15-20 days. However, one patient became worsen to critical. With active treatment, he had turned back to severe type and still stayed in hospital. Due to the CT finding at early stage, we could detect the changes in lung and perform active treatment as early as possible, which effectively shortened the duration of patients in severe condition. For patients who had unilateral glass-grinding change by CT scan at 3 days post-admission, oxygen inhalation and active symptomatic treatment were given to timely prevent the transition of mild disease to severe disease. For patients who were negative in coronavirus nucleic acid test after antiviral therapy for long time, we collected their blood serum and stem cells at the recovery stage. As for February 27, the accumulative number of discharge patients was 161. The cure rate was 67.6%. The average length of hospital stay was 12.5 days. Among cities which had accumulative confirmed COVID-19 patients of more than 200 cases, Changsha’s discharge rate ranks 5th.
1.2 For severe and critical patients, their condition changed rapidly and they had more basic diseases. Therefore, the treatment was more difficult than mild patients. In this case, we centralized our medical recourses, experts, drugs and patients. All severe and critical patients were admitted in two ICU wards, and all medical professionals experienced in intensive medicine were concentrated in these two wards. We adopted the ‘one-person-one-team’ strategy to secure every severe or critical patient to have his/her own team of doctor and nurse. Every day, the team leader must report all the patient’ situation to the senior doctors, including the vital signs, blood gas analysis results, changes in biochemical indexes and clinical symptoms, and airway management, etc. For patient who poorly responded to treatment, the onsite senior doctors need to provide alternative effective options as soon as possible. For patients who had basic diseases or complications, senior specialists would give their corresponding treatment advice. For patients who might became severe or critical according to image and laboratory alert, a group of senior experts would be invited through remote consultation system for next treatment regimen. Our senior experts were from three Xiangya affiliated hospitals, Hunan University of traditional Chinese Medicine, and Hunan Institute of traditional Chinese Medicine, etc.
1.3 As for the traditional Chinese medicine (TCM), more than 90% cases received TCM treatment. TCM experts differentiated symptoms and exerted treatment for patients daily. We found that COVID-19 in Changsha area had some regularity in TCM pathogenesis, which belonged to the ‘warm heat’ type of epidemic disease. On the whole, it could be treated according to TCM ‘warm’ epidemic disease; but there was also a great degree of variability, especially for patients with basic disease, old patients, and severe / critical patients. The TCM syndrome type of COVID-19 was closely related to its basic constitution, which accorded with the theory that "the external evil is moving, the recipient is hard to know; patient being aware once having symptoms, then disease could be distinguished ". From the real-world observation, among COVID-19 patient with mild and general type, TCM syndrome types ‘warm evil attacked defense system’, ‘warm dryness injured saliva’, and ‘little sun stagnated heat’ were common, and each syndrome type was also always coupled with ‘dampness evil (or turbid poison)’. For severe patients, common TCM syndrome types were ‘gas-water deficiency’, ‘evil heat blocked lung’, and ‘heat phlegm accumulated in lung’. For critical patients, the syndrome type and performance were ‘extreme gas-water deficiency’, ‘internal closed with external collapsed’.
1.4 Nutrition support and early rehabilitation training were important for critical patients. Nasal jejuna nutrition-feeding tube could effectively reduce the risk of reflux and aspiration, and improve the tolerance of patients to enteral nutrition (EN). Early rehabilitation training has pretty high potency ratio, because it could reduce the mortality of severe patients and shorten the length of hospital stay and length of ventilator use. But critical patients were not able to rehabilitate actively, so medical staff need to intervene proactively. COVID-19 patients, especially the severe patients, can achieve good outcome by early lung rehabilitation. Early lung rehabilitation (ELR) is good for sputum drainage and functional exercise of diaphragm; ELR can prevent thrombosis, re-infection and other complications; it is also conducive to control pneumonia, prevent ventilator-associated pneumonia, reduce the risk of deep venous thrombosis, and improve mental health and life quality.
1.5 Psychological care is particularly important in severe patients and those with positive viral nucleic acid for long time. On the one hand, they are concerned that the disease cannot be effectively controlled; on the other hand, they are concerned about the medication-caused side effects and sequelae after discharge. Most of these patients are highly educated and are more stressed than the average, so psychological care is particularly important. The measures we take are to send them daily greeting messages to relieve their psychological stress, eliminate their fear and improve their compliance with medication.
2. The second strategy is the infection control strategy. We have taken the following measures to prevent infection of medical workers:
2.1. We strictly set up individual ‘three zones’ (contaminated zone, potential contaminated zone, and clean zone) and ‘two channels’ (medical personnel passage and patient passage). All items must be passed through the transfer window, which is sterilized by ultraviolet light.
2.2 We setup dressing mirror for workers to check protective cloth by themselves. We also have full-time supervisor to double check the guard suite. In the clothes taking-off room, the clothes taking-off process is printed out on the wall, and surveillance cameras monitor the taking-off process. Medical workers who are going to leave the contaminated zone should be taken out in pairs for mutual supervision. Medical workers must bathe and change clothes before leaving the ward. Then, they stay in a designated hotel to rest.
2.3 Sufficient rest time and psychological care are necessary for medical workers. All medical staffs work 4 to 6 hours per shift. Anyone who has physical discomfort must leave the isolation ward and take a rest at the designated hotel. There are ‘three not-allowed’: 1) sick personnel is not allowed to work in isolation ward, 2) fatigue ones are not allowed to work, 3) workers without correct dressing are not allowed to work. Professional psychological counselors carry on psychological counseling for medical workers in designated hospital to relieve their panic mental.
2.4 To ensure the personal protection of medical workers who take care of patients during transporting, all patient-transporting vehicles are negative pressure ambulances.
3. The third one is the material support strategy. As shown in Figure 3, we have a strong material support system, including the net-work support system. To ensure the treating capacity of 300 patients, we renovated three floors in two buildings and opened eight nursing unit within 6 days immediately after Spring Festival. All the patients in Changsha area are timely admitted and treated in our hospital. All related departments, including the Finance Bureau, Health Commission, Residential and Construction Bureau, Environmental Protection Department, Gas Provider, Bureau of Governmental Affairs, CDC, etc, have made their best to contribute and ensure the hospitalization of all infected patients and zero-hospital infection of medical staff. In short period after COVID-19 outbreak, we selected and trained 600 medical staffs from the public hospitals throughout the city. We arranged them to work in isolation ward by stages and in groups. We also purchased all the protective materials and medical equipment in emergency, including ECMO, broncho-fiberscope, mobile CT, etc. We requisitioned three hotels for medical staffs to take a rest, and two hotels to centralize the discharged patients for isolation and clinical observation. To secure enough rest for medical staffs, nine buses are responsible for the daily shifting, according to the medical staffs’ working time schedule. Bureau of Environmental Protection and CDC are in charge of properly dealing with the medical sewage and trash. The gas, electricity, water and telecom providers ensure the sufficient resource supply. Governmental Affair Bureau guarantees the daily diet and nutrition of all medical staffs and patients. During the entire medical treatment process, it is precisely because of such a safeguard support system, we have no worries, and we spend all our time and energy on how to rescue, treat and care patients, how to do a good job for personal protection and prevent infection for workers. We make our best to control mild patients not to become severe, severe patients not to become critical, and critical patients not to die.
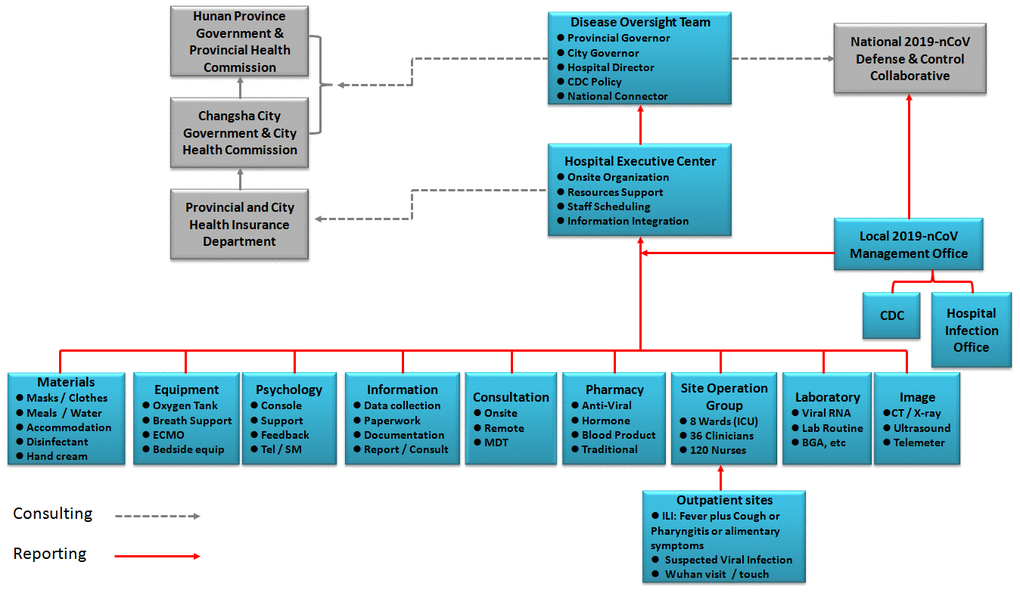
Figure 3. Organization structure of COVID-19 defense and control system.
As of February 27, 2020, two patients have died. One 64-year old male patient died on February 15, 2020. This patient had hypertension, COPD and smoking history. Multilobular infiltration, lymphopenia and bacterial co-infection occurred during disease progression. This patient had all six indexed in the MuLBSTA score [7], which is effective in predicting mortality in viral pneumonia. Another 58-year old male patient died on February 21, 2020. This patient left Wuhan on January 14, 2020, and was diagnosed and admitted on January 23, 2020. At admission, this patient had lung infiltration by CT scan, belonging to general type. On January 31, 2020, the disease progressed rapidly and critically. After 16-days of treatment, with invasive ventilation CRRT and even ECMO, this patient died on February 17, 2020.