Baseline characteristics
Of the 9570 participants included for analysis, the number of participants in good, intermediate and poor sleep quality group was 3703 (38.7%), 3863 (40.4%), and 2004 (20.9%) respectively (Figure 1). Mean age of our study cohort was 64.38 years, and the proportion of female was 57.1%. The proportion of female was highest in poor quality group (70.8%), followed by intermediate (57.6%) and good quality (49.2%) group. The proportion of depression symptom was also highest in poor quality group (10.4%), followed by intermediate group (3.0%) and good quality group (1.0%). Compared with good quality or intermediate quality group, poor quality group were less likely to drink alcohol greater than once a week, and less likely to have physical activities. The proportion of participants with prior hypertension increased progressively as sleep quality decreased (good, intermediate and poor sleep quality: 46.1%, 48.5% and 49.0%, respectively). Similarly, the proportion of participants with prior diabetes increased progressively as sleep quality decreased (good, intermediate and poor sleep quality: 12.5%, 14.1% and 15.0%, respectively).
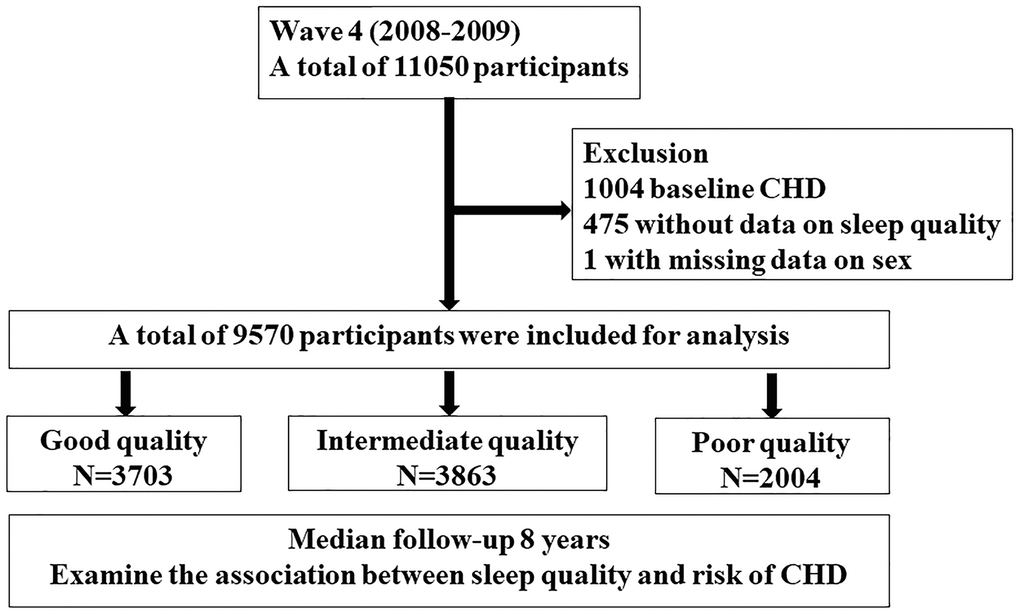
Figure 1. Study flow chart A total of 11050 participants from English longitudinal study of ageing cohort in wave 4 (2008-2009) were screened. After exclusion of participants with coronary heart disease at baseline, with missing data on sleep quality and sex, a total of 9570 participants were included for analysis. Participants were divided into three groups according to sleep quality and followed up over 8 years.
No significant difference in wealth, marital status, education level, NS-SEC classification, BMI, medical history of high cholesterol, chronic obstructive pulmonary disease and cancer were found across groups (Table 1).
Table 1. Baseline characteristics according to sleep quality.
| Variable | Good Quality N=3703 | Intermediate Quality N=3863 | Poor quality N=2004 | P value |
| Age (years) | 64.5±10.3 | 64.9 ±10.0 | 63.2±9.8 | <0.001 |
| Women (%) | 1822 (49.2) | 2224 (57.6) | 1418 (70.8) | <0.001 |
| Wealth quintile (%) | | | | 0.201 |
| 1 (lowest) | 548 (17.1) | 627 (18.7) | 313 (18.1) | |
| 2 | 646 (20.2) | 630 (18.8) | 366 (21.1) | |
| 3 | 642 (20.0) | 649 (19.3) | 3587 (20.7) | |
| 4 | 654 (20.0) | 727 (21.7) | 341 (19.7) | |
| 5 (highest) | 715 (22.3) | 725 (21.6) | 356 (20.5) | |
| NS-SEC classification (%) | | | | 0.622 |
| 1 | 1028 (31.9) | 1018 (30.3) | 548 (31.7) | |
| 2 | 794 (24.6) | 842 (25.1) | 412 (23.8) | |
| 3 | 1402 (43.5) | 1495 (44.6) | 768 (44.4) | |
| Education* (%) | | | | 0.246 |
| ≥NVQ3/GCE A level | 1518 (41.0) | 1579 (40.9) | 779 (38.9) | |
| Marital status (%) | | | | 0.361 |
| First and the only marriage | 2077 (56.1) | 2122 (54.9) | 1087 (54.2) | |
| BMI (kg/m2) | 27.3±7.1 | 27.4±7.4 | 26.9±7.6 | 0.122 |
| Depression symptoms (%) | 34 (1.0) | 96 (3.0) | 126 (10.4) | <0.001 |
| Current smoking (%) | 514 (15.5) | 472 (13.9) | 392 (22.1) | <0.001 |
| At least one alcoholic drink/week (%) | 2133 (66.5) | 2157 (63.9) | 876 (52.0) | <0.001 |
| At least one moderate activity/week (%) | 3004 (81.1) | 3053 (79.0) | 1309 (65.3) | <0.001 |
| Hypertension (%) | 1708 (46.1) | 1873 (48.5) | 982 (49.0) | 0.049 |
| Diabetes (%) | 461 (12.5) | 545 (14.1) | 300 (15.0) | 0.017 |
| High cholesterol (%) | 1206 (32.6) | 1248 (32.3) | 632(31.5) | 0.725 |
| COPD (%) | 95 (2.6) | 175(4.5) | 138 (6.9) | <0.001 |
| Cancer (%) | 168 (4.5) | 197 (5.1) | 107(5.3) | 0.337 |
| NS-SEC: national statistics social-economic classification;1: managerial and professional occupations; 2: Intermediate occupations; 3: routine and manual occupations; NVQ: National Vocational Qualification; GCE: General Certificate of Education; CSE: Center for Continuing Education; BMI: body mass index; COPD: chronic obstructive pulmonary disease. |
| *education: NVQ3/GCE A level is equivalent to senior high school. |
Sleep quality and outcome
A total of 411 (4.3%) incident cases occurred at a median 8-year follow-up. The number (incidence) of incident CHD cases in good, intermediate and poor quality groups was 128 (3.5%), 174 (4.5%) and 109 (5.4%), respectively. After simple adjustment of age and sex (model 1), the risk of CHD increased progressively with decreased sleep quality (Table 2). Compared with good quality group, HR (95% CI) for intermediate quality group was 1.331 (1.059, 1.674), for poor quality group was 2.001 (1.542, 2.596). Further adjustment of social-economic status, life style and conventional CHD risk factors did not significantly alter the association. Compared with good quality group, HR (95% CI) for intermediate quality group was 1.393 (1.005, 1.931), for poor quality group was 1.913 (1.206, 3.035). When the sleep quality score was modeled as continuous variable, one score increase was significantly associated with increased risk of CHD in all three models (Table 2).
Table 2. Association between baseline sleep quality with risk of CHD.
| Categorical | Continuous |
| Good Quality N=3703 | Intermediate Quality N=3863 | Poor quality N=2004 | Per one score increase |
| No. of Cases /Person-Years | 128/22596 | 174/24090 | 109/11824 | 411/58510 |
| Model 1 | 1 (Reference) | 1.331 (1.059, 1.674) | 2.001 (1.542, 2.596) | 1.444 (1.279, 1.630) |
| P value | | 0.014 | <0.001 | <0.001 |
| Model 2 | 1 (Reference) | 1.296 (0.998, 1.684) | 1.889 (1.399, 2.553) | 1.431 (1.243, 1.646) |
| P value | | 0.052 | <0.001 | <0.001 |
| Model 3 | 1 (Reference) | 1.393 (1.005, 1.931) | 1.913 (1.206, 3.035) | 1.502 (1.209, 1.865) |
| P value | | 0.047 | 0.006 | <0.001 |
| Model 1: adjusted for age, sex |
| Model 2: model 1+education, social economic classification, marital status, income |
| Model 3: model 2+ current smoking, alcohol consumption, BMI, physical activity, diabetes, high blood cholesterol, hypertension, depression, sleep duration |
The association between baseline sleep quality with secondary outcome are shown in Supplementary Tables 1 and 2, respectively. In all three models, the risk of angina increased progressively as sleep quality decreased. Regarding MI, intermediate quality group had a trend towards higher risk of MI compared with good quality group, but the association was not significant in all three models. Poor quality group had a significant higher risk of MI after adjustment of age and sex (model 1) and socio-economic factors (model 2), and a trend towards higher risk of MI after further adjustment of conventional CHD risk factors plus sleep duration (model 3, Supplementary Table 2).
The distribution of sleep quality score change between wave 4 and wave 6 are shown in Supplementary Figure 1. Approximately 90% of participants had a change less than or equal to 1 point, which indicated that a majority of participants in our study did not show a significant change in sleep quality during the first 4 years. Compared with maintaining good sleep quality between wave 4 and wave 6, maintaining intermediated sleep quality, and quality worsened was associated with trend towards higher CHD risk, and maintaining poor quality was associated with significant higher CHD risk in fully adjusted model (HR: 1.876, 95% CI: 1.055, 3.334, Supplementary Table 3). No obvious trend or significant association was found for sleep quality improved (HR: 0.992, 95% CI: 0.606, 1.624).
We also evaluated the association between the frequency of each sleep problem and risk of CHD (Supplementary Table 4). We have studied three sleep problems: difficulty falling asleep and wake up several times at night and wake up feeling tired and worn out. Regarding difficulty falling asleep, compared with patients who did not report the problem during the last month, those reported “three or more times a week” had higher risk of CHD (HR: 1.843, 95% CI: 1.166, 2.913, p=0.009). Similarly, participants who reported “wake up several times at night” three or more times a week had higher risk of CHD (HR: 1.710, 95% CI: 1.153, 2.538, p=0.008). Regarding “wake up feeling tired and worn out”, a frequency of “once or twice a week” (HR: 1.570, 95% CI: 1.022, 2.412, p=0.039) and “three or more times a week” (HR: 1.921, 95% CI: 1.280, 2.881, p=0.002) was associated with increased CHD risk.
In order to assess whether sleep quality improved the predictive performance of a tradition risk score, we compared the C-statistics between the traditional Framingham 10-year CVD risk score, and traditional+sleep risk score (new risk score). Framingham 10-year CVD risk score was developed based on age, sex, diabetes status, smoking status, treated or untreated systolic blood pressure, and blood lipids to predict 10-year CVD risk in the Framingham study [9]. C statistics for the new and traditional risk score was 0.66 and 0.65, respectively (C-statistics difference: 0.01, 95% CI: 0.0004-0.03, p=0.04, Supplementary Figure 2). Integrated Discrimination Improvement (IDI) was 0.003 (95% CI: 0.002, 0.005, P<0.001) and Net Reclassification Improvement (NRI) was 0.203 (95% CI: 0.095,0.311, P<0.001).
Subgroup and sensitivity analysis
Subgroup analysis showed sleep quality-CHD risk association did not differ significantly according to age, sex or depression symptoms (P interaction: 0.322 for age; 0.783 for sex, 0.657 for depression symptom respectively Table 3). In each age subgroup, poor sleep quality had a trend towards higher risk of CHD compared with good sleep quality. A similar trend was found in male, female, depression or no depression subgroup.
Table 3. Association between baseline sleep quality and risk of coronary according to age, sex and depression.
| Good quality | Intermediate quality | Poor quality | P interaction |
| Age | | | | 0.322 |
| <60 (N=3462) | 1 (Reference) | 1.007 (0.497, 2.043) | 1.433 (0.598, 3.433) | |
| [60-70) (N=3278) | 1 (Reference) | 2.000 (1.110, 3.603) | 2.192 (1.000, 4.804) | |
| [70-80) (N= 2027) | 1 (Reference) | 1.158 (0.685, 1.957) | 1.449 (0.655, 3.202) | |
| ≥80 (N=803) | 1 (Reference) | 1.905 (0.619, 5.866) | 5.837 (1.740, 19.576) | |
| Sex | | | | 0.783 |
| Male (N=4106) | 1 (Reference) | 1.315 (0.878, 1.970) | 1.665 (0.873, 3.176) | |
| Female (N=5464) | 1 (Reference) | 1.562 (0.897, 2.719) | 2.246 (1.177, 4.285) | |
| Depression symptom | | | | 0.657 |
| Yes (N=256) | 1 (Reference) | 1.466 (0.150, 14.326) | 1.010 (0.103, 9.869) | |
| No (N=7570) | 1 (Reference) | 1.385 (0.995, 1.927) | 2.004 (1.255, 3.199) | |
| adjusted for age, sex, education, social economic classification, marital status, income, current smoking, alcohol consumption, BMI, physical activity, diabetes, high blood cholesterol, hypertension, depression, sleep duration |
To reduce the effect of missing data, we used multiple imputation and calculated the HR (95% CI) for each outcome in the imputed dataset (Supplementary Table 5). Results in the imputed dataset were general consistent with the main analysis. Compared with good sleep quality, intermediate quality (HR: 1.385, 95% CI:1.028, 1.864, p < 0.001) and poor quality (HR: 1.945, 95% CI: 1.285, 2.943, p < 0.001) was associated with increased CHD risk, which was mainly driven by increased angina risk but not MI.
Since sleep duration is closely related to sleep quality, we also examined the effect of sleep quality on CHD risk in participants with normal sleep duration. Sensitivity analysis was performed by excluding participants with too short (<6 hours) or too long sleep (>9 hours). Poor sleep quality was associated with higher CHD risk than good sleep quality in fully adjusted model (HR: 2.058, 95% CI: 1.230, 3.444, p=0.006). Per one score increase was associated with 54.2% increased risk in CHD (Table 4).
Table 4. Association between baseline sleep quality with risk of CHD in participants with normal sleep duration (6–9 hours).
| Categorical | Continuous |
| Good Quality N=3466 | Intermediate Quality N=3397 | Poor quality N=1168 | Per one score increase |
| No. of Cases /Person-Years | 120/21292 | 150/21370 | 57/6970 | 327/49632 |
| Model 1 | 1 (reference) | 1.313 (1.032, 1.671) | 1.813 (1.316, 2.498) | 1.416 (1.216, 1.648) |
| P value | | 0.027 | <0.001 | <0.001 |
| Model 2 | 1 (reference) | 1.239 (0.940, 1.634) | 1.654 (1.139, 2.403) | 1.364 (1.143, 1.628) |
| P value | | 0.129 | 0.008 | <0.001 |
| Model 3 | 1 (reference) | 1.353 (0.958, 1.911) | 2.058 (1.230, 3.444) | 1.542 (1.212, 1.962) |
| P value | | 0.086 | 0.006 | <0.001 |
| Model 1: adjusted for age, sex |
| Model 2: model 1+education, social economic classification, marital status, income |
| Model 3: model 2+ current smoking, alcohol consumption, BMI, physical activity, diabetes, high blood cholesterol, hypertension, depression, sleep duration |