Introduction
Stroke brings notable health burden all around the world. It is the second leading cause of death and disability-adjusted life-years (DALYs) globally (5.5 million deaths, 116.4 million DALYs in 2016), but the first leading cause of death and DALYs in China (1.79 million deaths, 38.6 million DALYs in 2016) [1–3]. With striking improvement of strategies in prevention and specialist stroke care, China has experienced a transition in the epidemiology of stroke [4]. Its downtrend of stroke mortality is on par with the global tendency [1, 5]. However, the incidence rate has increased over the years and continues to increase, which are on the contrary with the decline trend in most regions worldwide [1, 5, 6]. (Figure 1) With over 5.5 million new cases in 2016, China had the highest age-standardized incidence of stroke [1]. Moreover, the incidence rate increases by 8.3% annually, which leads to a dramatic growth in stroke prevalence and substantial burden for both patients and the health system [4, 6, 7]. The upward tendency of stroke incidence in China has become a severe health problem and urges the optimization of managements.
![Percentage change in age-standardized incidence rates of overall stroke in different countries, 1990-2016, extracted from a systematic analysis for the Global Burden of Disease Study 2016 [1].](/article/203096/figure/f1/large)
Figure 1. Percentage change in age-standardized incidence rates of overall stroke in different countries, 1990-2016, extracted from a systematic analysis for the Global Burden of Disease Study 2016 [1].
In this review, we adopt updated data to highlight several most potential aspects of stroke risks and preventions in China from a comprehensive and comparative perspective. In comparison to those in western countries, the current situation of hypertension, underdiagnosis of atrial fibrillation and unhealthy lifestyles in China are serious; the use of antihypertensive therapy and anticoagulant therapy are insufficient in China. However, these approaches represent promising opportunities to decrease stroke incidence in China, if progress towards their wide-scale implementation are achieved. Besides, targeted antiplatelet regimes for different subpopulations and specific protections from cold waves will mitigate the morbidity of stroke. In addition, advanced knowledge for pathogenesis, identification and preventions of cancer-related stroke and recurrent stroke are required since their occurrence appears to be increasing in Chinese populations. Moreover, we introduce hypertension as a cause of stroke and a tentative concept of so-called stroke-prone status. Overall, our review is designed to provide guidance, insights and new information to patients, physicians, policymakers, and researchers aiming to decrease the increasing stroke incidence in China and other regions sharing similar situations including Southeast Asia and sub-Saharan Africa [1].
Serious situation of hypertension
Hypertension is viewed as the greatest modifiable risk factor for stroke generally [2, 4, 6, 8]. However, on the basis of animal experiments and epidemiological data displaying a strong association between hypertension and stroke, we conceive that hypertension can be viewed as more of a single cause of stroke than a risk factor. Firstly, high blood pressure was proven to be able to cause stroke pathologically in animal models via cerebral vascular remodeling, increased permeability, sclerosis of cerebral vessels and so on [9–12]. Then, large-scare surveys exhibited that over 84% of stroke patients had a history of hypertension when they were enrolled, and meanwhile, 71% of hypertensive patients in the Chinese population died of cerebral vascular accidents [8, 13, 14]. Moreover, the stronger association between hypertension and stroke in Chinese populations than in Whites corresponded to the severer situation of stroke [15–17]. Hypertension is associated with higher hazards in intracerebral hemorrhage (ICH), and consistently there were two fold proportion of ICH patients in China [15, 16]. The mean blood pressure was higher in China (130.0/76.4 mm Hg) than in America (125.1/72.5mm Hg) [18]. The severe blood pressure levels (≥160/100 mm Hg) were nearly 2.5 fold more common in China than in America [18]. When systolic blood pressure (SBP) elevated each 10mmHg, the risk of ischemic stroke (IS) increased about 30% and the risk of ICH increased about 60% in China [19], whereas the increase hazard of overall stroke was only about 20% in Whites [20]. Besides, not just in China, stronger association between hypertension and stroke was also revealed in regions sharing with elevated stroke incidence (e.g., Southeast Asia and Africa), on the evidence that their population-attributable risk (PAR) and odds ratio (OR) of hypertension for stroke exceeded that in western countries [16].
Albeit the awareness, treatment and control rates of hypertension among Chinese patients has dramatically increased, they are lower than that in western countries [7, 21]. For example, compared with the United State, China had considerably lower rates of hypertension awareness, treatment and control [18, 22]. (Figure 2) The greatest backwardness was the poor control of hypertension that might largely result from more common use of monotherapy antihypertensive drug regimens. In comparison to the monotherapy, single-pill combinations and multiple-pill combinations of antihypertensive drugs increased 55% and 26% likelihoods of better control of blood pressure, respectively [23]. However, merely 21.9% of Chinese hypertensive patients took multiple antihypertensive drugs in 2014 to 2017, while the percentage was up to 47.7% among American in 2009 to 2010 [22, 23]. About 81.5% of hypertensive patients that were treated but not controlled were those who received only one antihypertensive agent [22]. And equally, the remarkable achievement of hypertension control in America is now attributed to increasing use of multi-drug therapy [23].
![Comparisons among hypertensive patients between China and the USA during 2011 to 2012. SBPL: severe blood pressure levels (≥160/100 mm Hg). Percentage (%) in columns means: 1) SBPL: blood pressure of ≥160/100 mm Hg among hypertensive people (prevalence of severe hypertension among all people/prevalence of hypertension among all people). 2) Awareness: a self-reported physician diagnosis of hypertension or self-reported use of antihypertensive medication, among hypertensive people. 3) Treatment: self-reported use of antihypertensive medication, among hypertensive people. 4) Control: a mean systolic blood pressure of ≤140 mm Hg, and a mean diastolic blood pressure of ≤90 mm Hg, among people with previously diagnosed hypertension. Adapted from a study using data from CHARLS (China Health and Retirement Longitudinal Study, n=12654) and the NHANES (US National Health and Nutrition Examination Survey, n=2607) from 2011 to 2012 [18].](/article/203096/figure/f2/large)
Figure 2. Comparisons among hypertensive patients between China and the USA during 2011 to 2012. SBPL: severe blood pressure levels (≥160/100 mm Hg). Percentage (%) in columns means: 1) SBPL: blood pressure of ≥160/100 mm Hg among hypertensive people (prevalence of severe hypertension among all people/prevalence of hypertension among all people). 2) Awareness: a self-reported physician diagnosis of hypertension or self-reported use of antihypertensive medication, among hypertensive people. 3) Treatment: self-reported use of antihypertensive medication, among hypertensive people. 4) Control: a mean systolic blood pressure of ≤140 mm Hg, and a mean diastolic blood pressure of ≤90 mm Hg, among people with previously diagnosed hypertension. Adapted from a study using data from CHARLS (China Health and Retirement Longitudinal Study, n=12654) and the NHANES (US National Health and Nutrition Examination Survey, n=2607) from 2011 to 2012 [18].
Overall, hypertension might play a dominant role in stroke occurrence as a single direct cause and the inadequate use of antihypertension increases stroke onset related to uncontrolled hypertension. Rigorous interventions including but not limited to improving availability of antihypertensive medications and increasing prescription of high-value medications are required [24].
Underdiagnosis of atrial fibrillation and underuse of anticoagulants
Atrial fibrillation (AF) is associated with 5-fold risk for stroke and contributes to over 40% of stroke in patients older than 80 years [25, 26]. The excess risk of ischemic stroke due to AF was greater in China (OR 6.98, 95%CI 3.46- 14.1) than in Europe and America (OR 4.05, 95%CI 2.55-6.44) [16]. However, in the setting of increasing prevalence of AF internationally, the lowest prevalence of AF was estimated in China [16, 27, 28]. Compared with other risk factors, AF presented exceptionally lower prevalence in Chinese stroke patients than in white populations [15]. The prevalence of ischemic stroke with AF was about 10% while it was about 26~27% in Whites [29–32]. The gap lies more in the frequency of overlooked or underdiagnosed AF, rather than the low absolute number of patients [33]. This can be ascribed to the bulk of patients receiving 12-lead electrocardiography only. To enhance the identification and diagnosis is of significance since AF-related stroke can be prevented by initiating anticoagulation. Besides, a quarter of ischemic stroke is cryptogenic and a proportion of presumed cryptogenic transient ischemic attack (TIA) or stroke can be attributed to under-recognized atrial fibrillation [34–36]. And without recognized history of AF at discharge, stroke patients had 40% higher risk of stroke recurrence during one-year follow-up period [37]. Therefore, it is of necessity to intensify the detection of atrial fibrillation particularly transient paroxysmal and clinically silent AF. Advanced monitoring such as opportunistic or systematic screening, mobile cardiac outpatient telemetry and prolonged cardiac rhythm monitoring should be applied if appropriate [26, 33, 34, 38].
The use of oral anticoagulant therapy among new-onset AF patients in China was notably lower than that in other countries, and even failed to achieve the global average level [31, 39]. Even among stroke patients with non-valvular atrial fibrillation (NVAF), the utilization of anticoagulants was insufficient. Adjusted-dose warfarin and antiplatelet agents reduced stroke by 64% and 22%, respectively [40], but only 35.5% received warfarin but 62.7% received antiplatelet therapy among Chinese AF patients receiving antithrombotic therapy [41]. At discharge, merely 19.4% of stroke patients with NVAF in China received warfarin [32] whereas the proportion was 88% in America [42]. The underuse of warfarin mainly resulted from concern about higher bleeding risk in Asian population among doctors and patients [6, 32, 43]. Besides, owing to inadequate monitoring of INR and usage of diverse traditional Chinese herbals, about 55.2% of Chinese NVAF patients receiving warfarin did not reach the therapeutic range of INR [31]. New oral anticoagulants (NOAC), with superiority for stroke prevention, less side effects, fewer drug interactions and needlessness to surveil the INR, are better choices for Chinese patients [44]. However, only when NOAC are affordable will they be commonly used and their adherence be guaranteed. Overall, the underdiagnosis of AF combined with underuse of anticoagulants may cause an increase in stroke cases that could easily be prevented.
Unhealthy lifestyles
As a risk factor for hypertension and stroke, high sodium consumption was a serious issue in China [45, 46]. The intake of 8 to 9 g/d in the south and 12 to 18 g/d in the north entirely surpassed World Health Organization recommendation of 5g/d limit [46]. Salt and soy sauce are core condiments in Chinese Cuisine and salted food remain common in daily lives of rural people.
Current smoking conferred a PAR of 15% for stroke in China [16]. Even though the smoking prevalence and second-hand smoke exposure had reduced together with increasing percentage of ex-smokers over the years [47], Chinese was still the largest ethnic group of current smokers and made up a third of global male smoking populations [48]. The consumption of cigarettes in China was more than the combination of the next 40 highest consuming countries from 1970 to 2015, and continued to increase [49–51]. Furthermore, second-hand smoke exposure due to tobacco sucked in China brings larger hazards than that chewed in India where the number of smokers ranked second worldwide [49]. Ultimately, it may be very difficult to control tobacco use in China for several reasons. Tobacco is considered the third most addictive drugs to human [52], and there is also a widespread culture of use in China, where tobacco serves as a popular gift in traditional festivals to enhance relationships and a mediator to entertain clients in social intercourses.
Alcohol, another one of the top ten addictive drugs [52], is another risk factor for stroke especially intracerebral hemorrhage [15, 16]. Although the prevalence of weekly drinking decreased from 2004-2008 to 2013-2014, the mean alcohol consumption, drinking frequency and heavy episodic drinking prevalence are increasing in China, particularly among the young generation [53]. In the past three decades, the alcohol per-capita consumption has reduced in America and Europe, while it has risen in China [54, 55]. Similar to smoking, drinking alcohol especially strong spirits (e.g. Baijiu) is also a symbol of celebration and capacity in Chinese traditional culture [53, 55].
Driving motorcycles and private cars are also more attractive than walking and cycling to the Chinese, and these activities can exacerbate physical inactivity and increase exposure to air pollution, which are risk factors for stroke [6, 45]. Completely exceeding other regions, China presented the highest PAR (59.9%) of physical inactivity for stroke [16]. In addition, the concentration of PM2.5 in China was the second highest among 79 countries when studies showed that PM2.5 precipitated the incidence of stroke [6, 56].
Traditional, but less-healthy, lifestyles have existed in China for a long time, and many of these cultural living patterns may be at odds with modern approaches to stroke prevention [45]. Unhealthy lifestyles are increasingly common in younger generations of Chinese, which partly explains the younger onset of stroke in China than in other regions [4, 6, 15]. It is time to launch a nationwide campaign against the unhealthy lifestyles since they increase the occurrence of stroke. Advertising their hazards for health to the public, seeking for alternatives like salts with potassium chloride or magnesium sulfate, strengthening the price and excise tax of tobacco and alcohol, and increasing the use of clean fuels like gas and electricity are feasible actions [55, 57, 58]. Indeed, there are numerous opportunities for reducing stroke risk and improving health outcomes in China, however it may be difficult to change the rigid lifestyle patterns of the traditional Chinese culture which is contributing to the disease.
Antiplatelet therapy to be targeted
Valid antiplatelet drugs for primary prevention of stroke remain unclear. Taking aspirin daily was not beneficial for primary stroke prevention, but instead increased the risk of hemorrhagic stroke and gastrointestinal bleeding [59, 60]. Nevertheless, antiplatelet therapy plays a dominant role for the prevention of stroke recurrence and complications.
Aspirin, as the class 1 recommendation, was the first antiplatelet agent used for the secondary prevention of TIA and ischemic stroke. It decreases long-term risk of recurrent stroke by 13% and risk of early recurrent stroke by 60% [61]. Clopidogrel, a commonly prescribed and used antiplatelet agents, has greater effectiveness in stroke prevention and less side effects than aspirin [62]. The genetic polymorphisms of CYP2C19 account for the variable efficacy of this prodrug [63]. CYP2C19 loss-of-function allele (*2 and *3) carriers are poor metabolizers with reduced enzyme activity and an increased risk of composite vascular events [64]. Disappointingly, the frequency of such poor metabolizers was up to 58.8% among Chinese, which was overwhelmingly higher than that in Caucasians and African Americans [64, 65]. Dual antiplatelet therapies such as aspirin plus clopidogrel, aspirin plus dipyridamole, aspirin plus ticagrelor were superior to monotherapies in the therapeutic efficacy, but the frequency of bleeding events and discontinuation from trial medications increased, especially in Asian populations [66–69]. Hence, aspirin monotherapy is still the footstone for the prevention after stroke.
Although the effectiveness of antiplatelet regimes for stroke prevention have been demonstrated in large randomized controlled trials (RCT), it is not always applicable for every ethnic group that has divergent genetic profile. Although the utilization of antiplatelet agents in Chinese patients was always at a high level in different studies, this does not mean that the treatment functions consistently or side effects can be offset by efficacy [6]. Only by choosing targeted antiplatelet therapies for different subpopulations will benefits ensue maximally, especially when various antiplatelet regimes are emerging. Population-based investigations about options of different antiplatelet therapies pertaining to specific ethnic groups are required.
Prospect of recurrent stroke
Recurrent stroke accounts for over 20% of patients admitted to hospital with an acute stroke event [80, 81]. With worse outcomes in disability and fatality, recurrent stroke was at a frequent level and became more frequent than before in China while decline trends were showed in Sweden, Italy, and Scotland [82, 83]. For example, incidence of recurrent stroke in 2006-2012 was three times higher than that in 1992-1998 in rural China [83]. Nevertheless, updating data from large-scale observational studies that represent the whole population of China is needed.
The combination of the use of aspirin, smoking cessation, antihypertensive drugs, and statins reduced the risk of recurrent ischemic events by 75% [45]. In contrast, a recent international RCT(INSPiRE-TMS) yielded a partly divergent finding. Regardless of improved achievement of recommended secondary prevention targets in the long term, including blood pressure, LDL, physical activity and smoking cessation, a support programme for enhanced secondary prevention did not bring a significant reduction in major vascular events [81]. The conflict between studies otherwise reflects that towards risk factors, primary preventions for stroke count more than secondary preventions. Therefore, it makes sense that neglect of recent minor stroke or TIA, under-recognized of atrial fibrillation, inadequate antithrombotic therapies, and failure of long-term adherence to treatments precipitates the severity of recurrent stroke in China. Further studies are required to ascertain whether achieving the secondary prevention targets is beneficial to prevent recurrent stroke, and explore whether the targets should be more aggressive for those with a high risk of recurrence, whether there are more advanced interventions and whether it is necessary to positively detect stroke recurrence.
Concept of stroke-prone status
Stroke triggered by several conditions, encompassing acute infections, temperature decline and intensive unhealthy behaviors were elucidated in studies [89–92]. Solly Sebastian et al. revealed that the association between infection and stroke increased as their time interval shortened; A portion of patients had heavy alcohol intake within 24 hours preceding stroke onset; Moderate to extreme physical exertion tripled the risk of subarachnoid hemorrhage in the subsequent two hours [90–92]. However, exposure to similar triggers does not necessarily lead to similar outcome of stroke events, such as among the healthy population and certain patients with similar underlying diseases like hypertension or atrial fibrillation. Therefore, we presume that prior to the acute episode of stroke, there is a period when the internal environmental hemostasis is susceptible to outside attacks and is approaching the threshold of stroke onset. Then, when the host is exposed to triggers, critical inner pathophysiological changes provoke progressively, leading to an arrival of threshold and occurrence of subsequent stroke, which makes things change from quantity to quality. Herein, we call this period the stroke-prone status. It is a status when accumulation of inner changes is sufficient for triggers and is approaching the threshold of stroke onset (Figure 4).
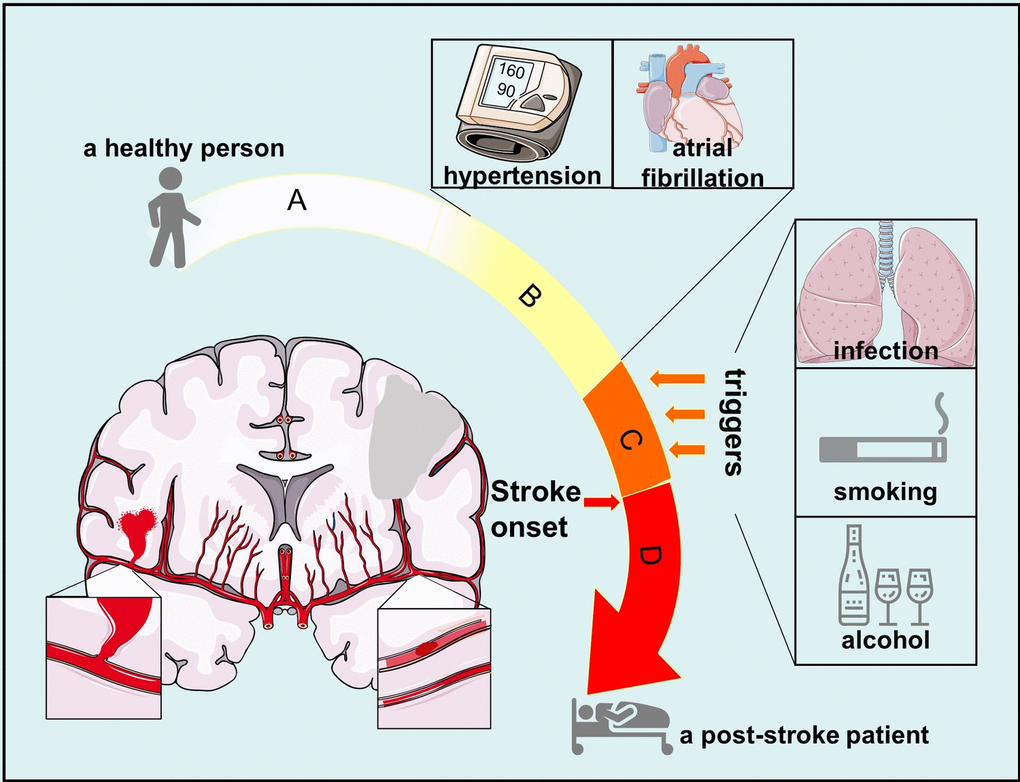
Figure 4. Process from normal status to post-stroke status. (A) normal status when a person is healthy and has no chronic disease; (B) status when a person suffers from diseases that are risk factors of stroke, including hypertension, atrial fibrillation and so on; (C) stroke-prone status when outside attacks such as infection and alcohol can trigger stroke onset in a person with risk factors of stroke; (D) post-stroke status when a person has suffered from stroke onset.
If individuals that are at the stroke-prone status suffer from triggers, subsequent stroke events are possible to occur. If individuals are at the stroke-prone status though they do not suffer from any triggers, internal environmental hemostasis changes at a low pace and stroke will not occur until the inner changes reach the threshold. For example, some patients suffer from stroke when they are sleeping. But if individuals are not at the stroke-prone status though they suffer from trigger conditions, stroke is less likely to occur, including the healthy population and patients with risk factors but not suffering from stroke in their whole lives. Additionally, animal experiments displayed that stroke prone Reno vascular hypertensive rats did not have stroke onsets until the fourth times of natural coldness [93]. This further suggested that there exists stroke-prone status before stroke onset and a threshold for stroke onset.
Regarding hypertension, there are periods of blood pressure higher than normal levels but not enough for hypertension diagnosis. Regarding diabetes, there is prediabetes called impaired glucose tolerance when blood sugar is higher than it should be but not enough to diagnose diabetes. Regarding acute myocardial infarction, there are conditions of coronary artery stenosis and angina lasting for some time. However, there are no periods identified before the acute onset of stroke, but it is essential for stroke prevention especially when stroke is still a heavy health burden with alarming incidence and prevalence. The identification of stroke-prone status can be a combination of clinical symptoms like fatigue, dizziness, malaise, experimental examinations like viscosity of blood, platelet reactivity, stenosis of cerebral vessels and thrombus in left atrium, and history of underlying diseases like duration of hypertension and atherosclerosis burden. Further research about details of stroke-prone status and threshold of stroke onset are required for exploration. If it is able to assess the stroke-prone status quantitatively and then appoint specific preventions at this period, large numbers of stroke incidence can be prevented.
Increase of the aging population
As the country with the highest population, China is facing with challenges of ascending rate of aging population. The Old Dependency Ratio in China (percent of 65-years and older to working ages) had increased from 9.9% in 2000 to 16.8% in 2018 [94], which was higher than the average ratio of the world (13.6% in 2018) [95]. This can be result from two of the three peak periods of population growth in 1950s to 1970s. A mass of babies born during those days are now entering their old age when stroke incidence is the highest among all age groups [8, 94].
In spite of China, aging has become a universal public problem in developed countries. Although aging is the irreversible risk factor of stroke, multiple modifiable health-related factors are concomitant in the elderly which should be paid more attention to. For example, the comorbidity with coronary heart disease, diabetes mellitus, dyslipidemia, mood or sleep disorders, physical inactivity and so on is common in the elderly. These factors all predispose elderly to higher risk of stroke. However, awareness and management of these aging-related comorbidities was less satisfying in China than those in developed countries [6, 16, 18, 45].
Conclusions
The increasing stroke incidence in China in contrast to the global trend has brought alarming and ascending burden to the health system. In this review, we discuss several of the most prominent causes of stroke facing the Chinese, and we highlight several opportunities to reduce stroke incidence through public outreach and education. Firstly, several unsolved aspects showing stronger associations with stroke occurrence in China have marked deficiencies in comparison to those in western countries. Hypertension is serious issue in China, among which the greatest challenges is reduced control of hypertension compared to other developed nations, due to the less frequent use of multiple antihypertensive medications. The underdiagnosis of atrial fibrillation and underuse of anticoagulants are much more common. Unhealthy lifestyles as parts of traditional cultures for years are still severe health issues. Secondly, targeted antiplatelet therapies for different subpopulations as well as protections from cold wave and preventions from weather-related stroke will further allay the stroke occurrence. Thirdly, the frequency of recurrent stroke is high and is increasing but, secondary prevention strategies aimed to reduced recurrent stroke remain elusive and related clinical trials are sparse. Cancer-related stroke also appears to be increasing but, advanced interventions and related research are limited. Finally, we introduce two perspectives: high blood pressure viewed as a direct cause of stroke; and a tentative concept called stroke-prone status. If individuals with risk factors are at stroke-prone status, they are susceptible to triggers and approaching the subsequent stroke onset.
In order to alleviate the stroke incidence in China, education is of paramount significance to increase individuals’ awareness of health. It is important to emphasize healthy lifestyles, adherence to drug therapies and protections from environmental events to the public, especially among the young generation and patients in rural areas. Physicians should enhance the diagnosis and treatment of hypertension and atrial fibrillation, formulate individualized regimes of antithrombotic drugs and provide more supports to patients under high risk of stroke. Policymakers should enforce vigorous policies for tobacco and alcohol cessation, carry out regional strategies to protect citizens from climate changes and increase health care expenditures. Further research is required to focus on aspects with limited advances, comprising recurrent stroke, cancer-related stroke and stroke-prone status. Details of the stroke-prone status and preventions inflicted at this stage remain to be explored.
We hope that aspects reflected in this review will inspire improved stroke awareness and prevention in countries facing an upward trend and high rates of the disease, similar to China. The odd ratios of hypertension, atrial fibrillation and alcohol intake for stroke in Southeast Asia and Africa are consistently higher than those in western countries [16]. The prevalence of smoking and drinking as well as the tobacco and alcohol consumption are at an overwhelmingly high level in Southeast Asian countries, particularly in Indonesia and Philippines where the policy of tobacco and alcohol is as weak as that in China [1, 48, 96]. With impact of extreme cold weathers due to Siberian cold current and declines of Arctic sea-ice, Mongolia that has the largest increase of stroke incidence worldwide and Russia that has completely high stroke incidence need to note the impact of cold waves to stroke as well [1, 97].
Collectively, aspects discussed above generated from the outlier (China) with increasing incidence of stroke are confronted with great challenges, but they are potential, modifiable and promising. Vigorous interventions and further research are expected from collaboration and efforts of different parts since primary prevention of stroke is the most cost-effective way to reduce the health burden.
Abbreviations
ACE: artificial cold exposure;
AF: atrial fibrillation;
DALYs: disability-adjusted life-years;
ICH: intracerebral hemorrhage;
INR: international normalized ratio;
IS: ischemic stroke;
NOAC: new oral anticoagulants;
NVAF: non-valvular atrial fibrillation;
OR: odds ratio;
PAR: population-attributable risk;
RCT: randomized controlled trial;
SBP: systolic blood pressure;
TIA: transient ischemic attack.
Author Contributions
XL, XR, YP designed the study. XL and HW wrote the initial draft of the manuscript. XR, HW and YP decided the final version of the manuscript. All authors contributed to the article and approved the submitted version.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Funding
This work was supported by The Chronic Noninfectious Disease Project of National Key R&D Program of China (2018YFC1314400, 2018YFC1314401) to Ying Peng. Partly also were supported by National Natural Science Foundation of China (81601042) and the Science and Technology Planning Project of Guangdong Province, China (No. 2014A020212090) to Hongxuan Wang.
References
-
1.
GBD 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019; 18:439–58. https://doi.org/10.1016/S1474-4422(19)30034-1 [PubMed]
-
2.
Feigin VL, Roth GA, Naghavi M, Parmar P, Krishnamurthi R, Chugh S, Mensah GA, Norrving B, Shiue I, Ng M, Estep K, Cercy K, Murray CJ, Forouzanfar MH, and Global Burden of Diseases, Injuries and Risk Factors Study 2013 and Stroke Experts Writing Group. Global burden of stroke and risk factors in 188 countries, during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016; 15:913–24. https://doi.org/10.1016/S1474-4422(16)30073-4 [PubMed]
-
3.
Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, Li X, Wang L, Wang L, Liu Y, Liu J, Zhang M, Qi J, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019; 394:1145–58. https://doi.org/10.1016/S0140-6736(19)30427-1 [PubMed]
-
4.
Guan T, Ma J, Li M, Xue T, Lan Z, Guo J, Shen Y, Chao B, Tian G, Zhang Q, Wang L, Liu Y. Rapid transitions in the epidemiology of stroke and its risk factors in China from 2002 to 2013. Neurology. 2017; 89:53–61. https://doi.org/10.1212/WNL.0000000000004056 [PubMed]
-
5.
Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, Moran AE, Sacco RL, Anderson L, Truelsen T, O’Donnell M, Venketasubramanian N, Barker-Collo S, et al, and Global Burden of Diseases, Injuries, and Risk Factors Study 2010 (GBD 2010) and the GBD Stroke Experts Group. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014; 383:245–54. https://doi.org/10.1016/s0140-6736(13)61953-4 [PubMed]
-
6.
Wu S, Wu B, Liu M, Chen Z, Wang W, Anderson CS, Sandercock P, Wang Y, Huang Y, Cui L, Pu C, Jia J, Zhang T, et al, and China Stroke Study Collaboration. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019; 18:394–405. https://doi.org/10.1016/S1474-4422(18)30500-3 [PubMed]
-
7.
Hu Ss, Gao Rl, Liu Ls, Zhu Ml, WANG Wen WY, Zhaosu WU, Huijun LI, Dongfeng GU, Yuejin Y, Zhe Z, Weiwei C. Summary of the 2018 Report on Cardiovascular Diseases in China. Chinese Circulation Journal. 2019; 34:209–20.
-
8.
Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, Wang L, Jiang Y, Li Y, Wang Y, Chen Z, Wu S, Zhang Y, et al, and NESS-China Investigators. Prevalence, Incidence, and Mortality of Stroke in China: Results from a Nationwide Population-Based Survey of 480 687 Adults. Circulation. 2017; 135:759–71. https://doi.org/10.1161/CIRCULATIONAHA.116.025250 [PubMed]
-
9.
Arribas SM, Gordon JF, Daly CJ, Dominiczak AF, McGrath JC. Confocal microscopic characterization of a lesion in a cerebral vessel of the stroke-prone spontaneously hypertensive rat. Stroke. 1996; 27:1118–22. https://doi.org/10.1161/01.str.27.6.1118 [PubMed]
-
10.
Pires PW, Deutsch C, McClain JL, Rogers CT, Dorrance AM. Tempol, a superoxide dismutase mimetic, prevents cerebral vessel remodeling in hypertensive rats. Microvasc Res. 2010; 80:445–52. https://doi.org/10.1016/j.mvr.2010.06.004 [PubMed]
-
11.
Tang Y, Li X, Li Y, Shen Q, Rong X, Huang R, Peng Y. Renovascular hypertension causes cerebral vascular remodeling. Neural Regeneration Research. 2011; 6:1977–81.
-
12.
Zeng J, Zhang Y, Mo J, Su Z, Huang R. Two-kidney, two clip renovascular hypertensive rats can be used as stroke-prone rats. Stroke. 1998; 29:1708–13. https://doi.org/10.1161/01.str.29.8.1708 [PubMed]
-
13.
Liu M, Li Y, Liu S, Wang W, Zhou M. [Burden on blood-pressure-related diseases among the Chinese population, in 2010]. Zhonghua Liu Xing Bing Xue Za Zhi. 2014; 35:680–83. [PubMed]
-
14.
Liu L, Wang Z, Gong L, Zhang Y, Thijs L, Staessen JA, Wang J. Blood pressure reduction for the secondary prevention of stroke: a Chinese trial and a systematic review of the literature. Hypertens Res. 2009; 32:1032–40. https://doi.org/10.1038/hr.2009.139 [PubMed]
-
15.
Tsai CF, Anderson N, Thomas B, Sudlow CL. Comparing Risk Factor Profiles between Intracerebral Hemorrhage and Ischemic Stroke in Chinese and White Populations: Systematic Review and Meta-Analysis. PLoS One. 2016; 11:e0151743. https://doi.org/10.1371/journal.pone.0151743 [PubMed]
-
16.
O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, Rao-Melacini P, Zhang X, Pais P, Agapay S, Lopez-Jaramillo P, Damasceno A, Langhorne P, et al, and INTERSTROKE investigators. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016; 388:761–75. https://doi.org/10.1016/S0140-6736(16)30506-2 [PubMed]
-
17.
Eastwood SV, Tillin T, Chaturvedi N, Hughes AD. Ethnic Differences in Associations Between Blood Pressure and Stroke in South Asian and European Men. Hypertension. 2015; 66:481–88. https://doi.org/10.1161/HYPERTENSIONAHA.115.05672 [PubMed]
-
18.
Lu Y, Wang P, Zhou T, Lu J, Spatz ES, Nasir K, Jiang L, Krumholz HM. Comparison of Prevalence, Awareness, Treatment, and Control of Cardiovascular Risk Factors in China and the United States. J Am Heart Assoc. 2018; 7:e007462. https://doi.org/10.1161/JAHA.117.007462 [PubMed]
-
19.
Lacey B, Lewington S, Clarke R, Kong XL, Chen Y, Guo Y, Yang L, Bennett D, Bragg F, Bian Z, Wang S, Zhang H, Chen J, et al, and China Kadoorie Biobank collaborative group. Age-specific association between blood pressure and vascular and non-vascular chronic diseases in 0.5 million adults in China: a prospective cohort study. Lancet Glob Health. 2018; 6:e641–49. https://doi.org/10.1016/S2214-109X(18)30217-1 [PubMed]
-
20.
Staessen JA, Gasowski J, Wang JG, Thijs L, Den Hond E, Boissel JP, Coope J, Ekbom T, Gueyffier F, Liu L, Kerlikowske K, Pocock S, Fagard RH. Risks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trials. Lancet. 2000; 355:865–72. https://doi.org/10.1016/s0140-6736(99)07330-4 [PubMed]
-
21.
Wolf-Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR, Poulter N, Primatesta P, Stegmayr B, Thamm M. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004; 43:10–17. https://doi.org/10.1161/01.HYP.0000103630.72812.10 [PubMed]
-
22.
Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, Cheng X, Mu L, Zhang H, Liu J, Su M, Zhao H, Spatz ES, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet. 2017; 390:2549–58. https://doi.org/10.1016/S0140-6736(17)32478-9 [PubMed]
-
23.
Gu Q, Burt VL, Dillon CF, Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health And Nutrition Examination Survey, 2001 to 2010. Circulation. 2012; 126:2105–14. https://doi.org/10.1161/CIRCULATIONAHA.112.096156 [PubMed]
-
24.
Su M, Zhang Q, Bai X, Wu C, Li Y, Mossialos E, Mensah GA, Masoudi FA, Lu J, Li X, Salas-Vega S, Zhang A, Lu Y, et al. Availability, cost, and prescription patterns of antihypertensive medications in primary health care in China: a nationwide cross-sectional survey. Lancet. 2017; 390:2559–68. https://doi.org/10.1016/S0140-6736(17)32476-5 [PubMed]
-
25.
Piccini JP Sr, Fonarow GC. Preventing Stroke in Patients With Atrial Fibrillation-A Steep Climb Away From Achieving Peak Performance. JAMA Cardiol. 2016; 1:63–64. https://doi.org/10.1001/jamacardio.2015.0382 [PubMed]
-
26.
Zimetbaum P. Atrial Fibrillation. Ann Intern Med. 2017; 166:ITC33–48. https://doi.org/10.7326/AITC201703070 [PubMed]
-
27.
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim YH, McAnulty JH Jr, Zheng ZJ, Forouzanfar MH, Naghavi M, Mensah GA, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014; 129:837–47. https://doi.org/10.1161/CIRCULATIONAHA.113.005119 [PubMed]
-
28.
Rahman F, Kwan GF, Benjamin EJ. Global epidemiology of atrial fibrillation. Nat Rev Cardiol. 2014; 11:639–54. https://doi.org/10.1038/nrcardio.2014.118 [PubMed]
-
29.
McGrath ER, Kapral MK, Fang J, Eikelboom JW, Conghaile Aó, Canavan M, O’Donnell MJ, and Investigators of the Ontario Stroke Registry. Association of atrial fibrillation with mortality and disability after ischemic stroke. Neurology. 2013; 81:825–32. https://doi.org/10.1212/WNL.0b013e3182a2cc15 [PubMed]
-
30.
Hanchate AD, Schwamm LH, Huang W, Hylek EM. Comparison of ischemic stroke outcomes and patient and hospital characteristics by race/ethnicity and socioeconomic status. Stroke. 2013; 44:469–76. https://doi.org/10.1161/STROKEAHA.112.669341 [PubMed]
-
31.
Wang C, Yang Z, Wang C, Wang Y, Zhao X, Liu L, Wang DZ, Li H, Wang Y. Significant underuse of warfarin in patients with nonvalvular atrial fibrillation: results from the China national stroke registry. J Stroke Cerebrovasc Dis. 2014; 23:1157–63. https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.10.006 [PubMed]
-
32.
Yang X, Li Z, Zhao X, Wang C, Liu L, Wang C, Pan Y, Li H, Wang D, Hart RG, Wang Y, Wang Y, and China National Stroke Registry II Investigators. Use of Warfarin at Discharge Among Acute Ischemic Stroke Patients With Nonvalvular Atrial Fibrillation in China. Stroke. 2016; 47:464–70. https://doi.org/10.1161/STROKEAHA.115.011833 [PubMed]
-
33.
Yang X, Li S, Zhao X, Liu L, Jiang Y, Li Z, Wang Y, Wang Y. Atrial fibrillation is not uncommon among patients with ischemic stroke and transient ischemic stroke in China. BMC Neurol. 2017; 17:207. https://doi.org/10.1186/s12883-017-0987-y [PubMed]
-
34.
Tayal AH, Tian M, Kelly KM, Jones SC, Wright DG, Singh D, Jarouse J, Brillman J, Murali S, Gupta R. Atrial fibrillation detected by mobile cardiac outpatient telemetry in cryptogenic TIA or stroke. Neurology. 2008; 71:1696–701. https://doi.org/10.1212/01.wnl.0000325059.86313.31 [PubMed]
-
35.
Dalen JE, Alpert JS. Silent Atrial Fibrillation and Cryptogenic Strokes. Am J Med. 2017; 130:264–67. https://doi.org/10.1016/j.amjmed.2016.09.027 [PubMed]
-
36.
Gladstone DJ, Spring M, Dorian P, Panzov V, Thorpe KE, Hall J, Vaid H, O’Donnell M, Laupacis A, Côté R, Sharma M, Blakely JA, Shuaib A, et al, and EMBRACE Investigators and Coordinators. Atrial fibrillation in patients with cryptogenic stroke. N Engl J Med. 2014; 370:2467–77. https://doi.org/10.1056/NEJMoa1311376 [PubMed]
-
37.
Hsu CY, Singer DE, Kamel H, Wu YL, Chen PC, Lee JD, Lee M, Ovbiagele B. Unrecognized History of Transient Atrial Fibrillation at the Time of Discharge from an Index Stroke Hospitalization Is Associated with Increased Recurrent Stroke Risk. J Stroke. 2019; 21:190–94. https://doi.org/10.5853/jos.2018.03265 [PubMed]
-
38.
Orchard J, Lowres N, Neubeck L, Freedman B. Atrial fibrillation: is there enough evidence to recommend opportunistic or systematic screening? Int J Epidemiol. 2018; 47:1372–78. https://doi.org/10.1093/ije/dyy111 [PubMed]
-
39.
Steinberg BA, Gao H, Shrader P, Pieper K, Thomas L, Camm AJ, Ezekowitz MD, Fonarow GC, Gersh BJ, Goldhaber S, Haas S, Hacke W, Kowey PR, et al, and GARFIELD-AF, and ORBIT-AF Investigators. International trends in clinical characteristics and oral anticoagulation treatment for patients with atrial fibrillation: Results from the GARFIELD-AF, ORBIT-AF I, and ORBIT-AF II registries. Am Heart J. 2017; 194:132–40. https://doi.org/10.1016/j.ahj.2017.08.011 [PubMed]
-
40.
Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007; 146:857–67. https://doi.org/10.7326/0003-4819-146-12-200706190-00007 [PubMed]
-
41.
Sun Y, Hu D. Risk profiles and antithrombotic treatment of patients with atrial fibrillation in china: China registry of atrial fibrillation (CRAF). Circulation. 2013; 128.
-
42.
Xian Y, Wu J, O’Brien EC, Fonarow GC, Olson DM, Schwamm LH, Bhatt DL, Smith EE, Suter RE, Hannah D, Lindholm B, Maisch L, Greiner MA, et al. Real world effectiveness of warfarin among ischemic stroke patients with atrial fibrillation: observational analysis from Patient-Centered Research into Outcomes Stroke Patients Prefer and Effectiveness Research (PROSPER) study. BMJ. 2015; 351:h3786. https://doi.org/10.1136/bmj.h3786 [PubMed]
-
43.
Gao Q, Fu X, Wei JW, Chen X, Huang Y, Wang J, Anderson CS, Wong KS, and China QUEST Study Investigators. Use of oral anticoagulation among stroke patients with atrial fibrillation in China: the ChinaQUEST (Quality evaluation of stroke care and treatment) registry study. Int J Stroke. 2013; 8:150–54. https://doi.org/10.1111/j.1747-4949.2011.00716.x [PubMed]
-
44.
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, Camm AJ, Weitz JI, Lewis BS, Parkhomenko A, Yamashita T, Antman EM. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014; 383:955–62. https://doi.org/10.1016/S0140-6736(13)62343-0 [PubMed]
-
45.
Pandian JD, Gall SL, Kate MP, Silva GS, Akinyemi RO, Ovbiagele BI, Lavados PM, Gandhi DB, Thrift AG. Prevention of stroke: a global perspective. Lancet. 2018; 392:1269–78. https://doi.org/10.1016/S0140-6736(18)31269-8 [PubMed]
-
46.
Wong ND, Franklin SS. Reducing the Burden of Hypertension: China’s Long March Ahead. JAMA Intern Med. 2016; 176:532–33. https://doi.org/10.1001/jamainternmed.2016.0213 [PubMed]
-
47.
Li X, Galea G. Healthy China 2030: an opportunity for tobacco control. Lancet. 2019; 394:1123–25. https://doi.org/10.1016/S0140-6736(19)32048-3 [PubMed]
-
48.
GBD 2015 Tobacco Collaborators. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet. 2017; 389:1885–906. https://doi.org/10.1016/S0140-6736(17)30819-X [PubMed]
-
49.
Hoffman SJ, Mammone J, Rogers Van Katwyk S, Sritharan L, Tran M, Al-Khateeb S, Grjibovski A, Gunn E, Kamali-Anaraki S, Li B, Mahendren M, Mansoor Y, Natt N, et al. Cigarette consumption estimates for 71 countries from 1970 to 2015: systematic collection of comparable data to facilitate quasi-experimental evaluations of national and global tobacco control interventions. BMJ. 2019; 365:l2231. https://doi.org/10.1136/bmj.l2231 [PubMed]
-
50.
China Tobacco. Analysis of the national tobacco market in 2017. TOBACCO C. http://www.tobacco.gov.cn/html/56/86856369_n.html.
-
51.
Consumption issue of tobacco worldwide. Atlas TT. https://tobaccoatlas.org/topic/consumption/.
-
52.
Nutt D, King LA, Saulsbury W, Blakemore C. Development of a rational scale to assess the harm of drugs of potential misuse. Lancet. 2007; 369:1047–53. https://doi.org/10.1016/S0140-6736(07)60464-4 [PubMed]
-
53.
Im PK, Millwood IY, Guo Y, Du H, Chen Y, Bian Z, Tan Y, Guo Z, Wu S, Hua Y, Li L, Yang L, Chen Z, and China Kadoorie Biobank (CKB) collaborative group. Patterns and trends of alcohol consumption in rural and urban areas of China: findings from the China Kadoorie Biobank. BMC Public Health. 2019; 19:217. https://doi.org/10.1186/s12889-019-6502-1 [PubMed]
-
54.
Manthey J, Shield KD, Rylett M, Hasan OS, Probst C, Rehm J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: a modelling study. Lancet. 2019; 393:2493–502. https://doi.org/10.1016/S0140-6736(18)32744-2 [PubMed]
-
55.
Jiang H, Room R, Hao W. Alcohol and related health issues in China: action needed. Lancet Glob Health. 2015; 3:e190–91. https://doi.org/10.1016/S2214-109X(15)70017-3 [PubMed]
-
56.
Huang K, Liang F, Yang X, Liu F, Li J, Xiao Q, Chen J, Liu X, Cao J, Shen C, Yu L, Lu F, Wu X, et al. Long term exposure to ambient fine particulate matter and incidence of stroke: prospective cohort study from the China-PAR project. BMJ. 2019; 367:l6720. https://doi.org/10.1136/bmj.l6720 [PubMed]
-
57.
Zhou B, Webster J, Fu LY, Wang HL, Wu XM, Wang WL, Shi JP. Intake of low sodium salt substitute for 3years attenuates the increase in blood pressure in a rural population of North China - A randomized controlled trial. Int J Cardiol. 2016; 215:377–82. https://doi.org/10.1016/j.ijcard.2016.04.073 [PubMed]
-
58.
Hoffman SJ, Poirier MJ, Rogers Van Katwyk S, Baral P, Sritharan L. Impact of the WHO Framework Convention on Tobacco Control on global cigarette consumption: quasi-experimental evaluations using interrupted time series analysis and in-sample forecast event modelling. BMJ. 2019; 365:l2287. https://doi.org/10.1136/bmj.l2287 [PubMed]
-
59.
Judge C, Ruttledge S, Murphy R, Loughlin E, Gorey S, Costello M, Nolan A, Ferguson J, Halloran MO, O’Canavan M, O’Donnell MJ. Aspirin for primary prevention of stroke in individuals without cardiovascular disease-A meta-analysis. Int J Stroke. 2020; 15:9–17. https://doi.org/10.1177/1747493019858780 [PubMed]
-
60.
McCarthy M. FDA questions use of aspirin for primary prevention of stroke and heart attack. BMJ. 2014; 348:g3168. https://doi.org/10.1136/bmj.g3168 [PubMed]
-
61.
Rothwell PM, Algra A, Chen Z, Diener HC, Norrving B, Mehta Z. Effects of aspirin on risk and severity of early recurrent stroke after transient ischaemic attack and ischaemic stroke: time-course analysis of randomised trials. Lancet. 2016; 388:365–75. https://doi.org/10.1016/S0140-6736(16)30468-8 [PubMed]
-
62.
CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee. Lancet. 1996; 348:1329–39. https://doi.org/10.1016/s0140-6736(96)09457-3 [PubMed]
-
63.
Simon T, Verstuyft C, Mary-Krause M, Quteineh L, Drouet E, Méneveau N, Steg PG, Ferrières J, Danchin N, Becquemont L, and French Registry of Acute ST-Elevation and Non-ST-Elevation Myocardial Infarction (FAST-MI) Investigators. Genetic determinants of response to clopidogrel and cardiovascular events. N Engl J Med. 2009; 360:363–75. https://doi.org/10.1056/NEJMoa0808227 [PubMed]
-
64.
Wang Y, Zhao X, Lin J, Li H, Johnston SC, Lin Y, Pan Y, Liu L, Wang D, Wang C, Meng X, Xu J, Wang Y, and CHANCE investigators. Association Between CYP2C19 Loss-of-Function Allele Status and Efficacy of Clopidogrel for Risk Reduction Among Patients With Minor Stroke or Transient Ischemic Attack. JAMA. 2016; 316:70–78. https://doi.org/10.1001/jama.2016.8662 [PubMed]
-
65.
Dean L. Clopidogrel Therapy and CYP2C19 Genotype.. In: Pratt VM, Scott SA, Pirmohamed M, Esquivel B, Kane MS, Kattman BL, Malheiro AJ, editors. Medical Genetics Summaries. Bethesda (MD): National Center for Biotechnology Information (US); 2012. [PubMed]
-
66.
Wang Y, Chen W, Lin Y, Meng X, Chen G, Wang Z, Wu J, Wang D, Li J, Cao Y, Xu Y, Zhang G, Li X, et al, and PRINCE Protocol Steering Group. Ticagrelor plus aspirin versus clopidogrel plus aspirin for platelet reactivity in patients with minor stroke or transient ischaemic attack: open label, blinded endpoint, randomised controlled phase II trial. BMJ. 2019; 365:l2211. https://doi.org/10.1136/bmj.l2211 [PubMed]
-
67.
Wang Y, Wang Y, Zhao X, Liu L, Wang D, Wang C, Wang C, Li H, Meng X, Cui L, Jia J, Dong Q, Xu A, et al, and CHANCE Investigators. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013; 369:11–19. https://doi.org/10.1056/NEJMoa1215340 [PubMed]
-
68.
Halkes PH, van Gijn J, Kappelle LJ, Koudstaal PJ, Algra A, and ESPRIT Study Group. Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial. Lancet. 2006; 367:1665–73. https://doi.org/10.1016/S0140-6736(06)68734-5 [PubMed]
-
69.
Greving JP, Diener HC, Reitsma JB, Bath PM, Csiba L, Hacke W, Kappelle LJ, Koudstaal PJ, Leys D, Mas JL, Sacco RL, Algra A. Antiplatelet Therapy After Noncardioembolic Stroke. Stroke. 2019; 50:1812–18. https://doi.org/10.1161/STROKEAHA.118.024497 [PubMed]
-
70.
Gao J, Yu F, Xu Z, Duan J, Cheng Q, Bai L, Zhang Y, Wei Q, Yi W, Pan R, Su H. The association between cold spells and admissions of ischemic stroke in Hefei, China: Modified by gender and age. Sci Total Environ. 2019; 669:140–47. https://doi.org/10.1016/j.scitotenv.2019.02.452 [PubMed]
-
71.
Li XP, He L, Wang YD, Li Y, Li M, Peng Y. Identification of potential biomarkers for artificial cold exposure-induced hypertensive stroke by proteomic analysis. J Stroke Cerebrovasc Dis. 2014; 23:2671–80. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.06.014 [PubMed]
-
72.
Morabito M, Crisci A, Vallorani R, Modesti PA, Gensini GF, Orlandini S. Innovative approaches helpful to enhance knowledge on weather-related stroke events over a wide geographical area and a large population. Stroke. 2011; 42:593–600. https://doi.org/10.1161/STROKEAHA.110.602037 [PubMed]
-
73.
Ma W, Xu X, Peng L, Kan H. Impact of extreme temperature on hospital admission in Shanghai, China. Sci Total Environ. 2011; 409:3634–37. https://doi.org/10.1016/j.scitotenv.2011.06.042 [PubMed]
-
74.
Rakers F, Schiffner R, Rupprecht S, Brandstädt A, Witte OW, Walther M, Schlattmann P, Schwab M. Rapid weather changes are associated with increased ischemic stroke risk: a case-crossover study. Eur J Epidemiol. 2016; 31:137–46. https://doi.org/10.1007/s10654-015-0060-3 [PubMed]
-
75.
Chak Ho H, Chan TC, Xu Z, Huang C, Li C. Individual- and community-level shifts in mortality patterns during the January 2016 East Asia cold wave associated with a super El Niño event: Empirical evidence in Hong Kong. Sci Total Environ. 2020; 711:135050. https://doi.org/10.1016/j.scitotenv.2019.135050 [PubMed]
-
76.
Protsiv M, Ley C, Lankester J, Hastie T, Parsonnet J. Decreasing human body temperature in the United States since the industrial revolution. Elife. 2020; 9:e49555. https://doi.org/10.7554/eLife.49555 [PubMed]
-
77.
Guo P, Zheng M, Wang Y, Feng W, Wu J, Deng C, Luo G, Wang L, Pan B, Liu H. Effects of ambient temperature on stroke hospital admissions: Results from a time-series analysis of 104,432 strokes in Guangzhou, China. Sci Total Environ. 2017; 580:307–15. https://doi.org/10.1016/j.scitotenv.2016.11.093 [PubMed]
-
78.
Luo Y, Li H, Huang F, Van Halm-Lutterodt N, Qin Xu, Wang A, Guo J, Tao L, Li X, Liu M, Zheng D, Chen S, Zhang F, et al. The cold effect of ambient temperature on ischemic and hemorrhagic stroke hospital admissions: A large database study in Beijing, China between years 2013 and 2014-Utilizing a distributed lag non-linear analysis. Environ Pollut. 2018; 232:90–96. https://doi.org/10.1016/j.envpol.2017.09.021 [PubMed]
-
79.
Huang R, Chen L, Liu B, Gao Q, Zeng J, Su Z. Prophylactic effect of batroxobin on stroke induced by cold current in hypertensive. Chinese journal of nervous and mental diseases. 2005; 2:104–07.
-
80.
Coull AJ, Rothwell PM. Underestimation of the early risk of recurrent stroke: evidence of the need for a standard definition. Stroke. 2004; 35:1925–29. https://doi.org/10.1161/01.STR.0000133129.58126.67 [PubMed]
-
81.
Ahmadi M, Laumeier I, Ihl T, Steinicke M, Ferse C, Endres M, Grau A, Hastrup S, Poppert H, Palm F, Schoene M, Seifert CL, Kandil FI, et al. A support programme for secondary prevention in patients with transient ischaemic attack and minor stroke (INSPiRE-TMS): an open-label, randomised controlled trial. Lancet Neurol. 2020; 19:49–60. https://doi.org/10.1016/S1474-4422(19)30369-2 [PubMed]
-
82.
Liu J, Zhao D, Wang W, Sun JY, Li Y, Jia YN. [Trends regarding the incidence of recurrent stroke events in Beijing]. Zhonghua Liu Xing Bing Xue Za Zhi. 2007; 28:437–40. [PubMed]
-
83.
Zhao W, Wu J, Liu J, Wu Y, Ni J, Gu H, Tu J, Wang J, An Z, Ning X. Trends in the incidence of recurrent stroke at 5 years after the first-ever stroke in rural China: a population-based stroke surveillance from 1992 to 2017. Aging (Albany NY). 2019; 11:1686–94. https://doi.org/10.18632/aging.101862 [PubMed]
-
84.
Navi BB, Iadecola C. Ischemic stroke in cancer patients: A review of an underappreciated pathology. Ann Neurol. 2018; 83:873–83. https://doi.org/10.1002/ana.25227 [PubMed]
-
85.
Zaorsky NG, Zhang Y, Tchelebi LT, Mackley HB, Chinchilli VM, Zacharia BE. Stroke among cancer patients. Nat Commun. 2019; 10:5172. https://doi.org/10.1038/s41467-019-13120-6 [PubMed]
-
86.
Kim JM, Jung KH, Park KH, Lee ST, Chu K, Roh JK. Clinical manifestation of cancer related stroke: retrospective case-control study. J Neurooncol. 2013; 111:295–301. https://doi.org/10.1007/s11060-012-1011-4 [PubMed]
-
87.
Zeng H, Chen W, Zheng R, Zhang S, Ji JS, Zou X, Xia C, Sun K, Yang Z, Li H, Wang N, Han R, Liu S, et al. Changing cancer survival in China during 2003-15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health. 2018; 6:e555–67. https://doi.org/10.1016/S2214-109X(18)30127-X [PubMed]
-
88.
Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, Bonaventure A, Valkov M, Johnson CJ, Estève J, Ogunbiyi OJ, Azevedo E Silva G, Chen WQ, et al, and CONCORD Working Group. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018; 391:1023–75. https://doi.org/10.1016/S0140-6736(17)33326-3 [PubMed]
-
89.
Fukuda H, Ninomiya H, Ueba Y, Ohta T, Kaneko T, Kadota T, Hamada F, Fukui N, Nonaka M, Watari Y, Nishimoto S, Fukuda M, Hayashi S, et al. Impact of temperature decline from the previous day as a trigger of spontaneous subarachnoid hemorrhage: case-crossover study of prefectural stroke database. J Neurosurg. 2019; 1:1–9. https://doi.org/10.3171/2019.4.JNS19175 [PubMed]
-
90.
Sebastian S, Stein LK, Dhamoon MS. Infection as a Stroke Trigger. Stroke. 2019; 50:2216–18. https://doi.org/10.1161/STROKEAHA.119.025872 [PubMed]
-
91.
Anderson C, Ni Mhurchu C, Scott D, Bennett D, Jamrozik K, Hankey G, and Australasian Cooperative Research on Subarachnoid Hemorrhage Study Group. Triggers of subarachnoid hemorrhage: role of physical exertion, smoking, and alcohol in the Australasian Cooperative Research on Subarachnoid Hemorrhage Study (ACROSS). Stroke. 2003; 34:1771–76. https://doi.org/10.1161/01.STR.0000077015.90334.A7 [PubMed]
-
92.
Hillbom M, Numminen H, Juvela S. Recent heavy drinking of alcohol and embolic stroke. Stroke. 1999; 30:2307–12. https://doi.org/10.1161/01.str.30.11.2307 [PubMed]
-
93.
Huang R, Xiao X, Li L, Luo S, Gao Q, Huang H. Experimental study on the meteorological factors inducing the occurrence of stroke. Chinese journal of geriatrics. 2001; 20:45–47.
-
94.
National data. China NBoSo. http://data.stats.gov.cn/english/easyquery.htm?cn=C01. Accessed May 1.
-
95.
World Bank Open Data. Bank TW. https://data.worldbank.org/. Accessed January 15.
-
96.
Tang YL, Xiang XJ, Wang XY, Cubells JF, Babor TF, Hao W. Alcohol and alcohol-related harm in China: policy changes needed. Bull World Health Organ. 2013; 91:270–76. https://doi.org/10.2471/BLT.12.107318 [PubMed]
-
97.
Nandintsetseg B, Shinoda M, Du C, Munkhjargal E. Cold-season disasters on the Eurasian steppes: Climate-driven or man-made. Sci Rep. 2018; 8:14769. https://doi.org/10.1038/s41598-018-33046-1 [PubMed]