Study characteristics
Figure 1 presents the PRISMA flow diagram of this study. First, an initial search generated 2,992 potentially relevant papers, of which 2001 identified form Pubmed, and 991 from medRxiv or bioRxiv. After a number of screenings, 69 studies were identified (Supplementary Table 1). Of them, 67 (97.1%) reported Chinese COVID-19 patients, and 2 from either Japan or Singapore. The case number of each study ranged from 21 to 1780, with a mean of 218. The NOS score ranged from 5 to 7, which means a moderate methodological quality. Of the 69 publications, 2 duplicated studies (endpoints, exposure indicators and populations are completely covered by other studies), 4 studies with unique endpoints (survival ≤3d, refractory, liver injury, and time since symptom onset > 10 days), and 2 studies with different grouping methods for disease severity were excluded, which resulted that 61 studies were eventually eligible for the quantitative synthesis (Supplementary Table 1).
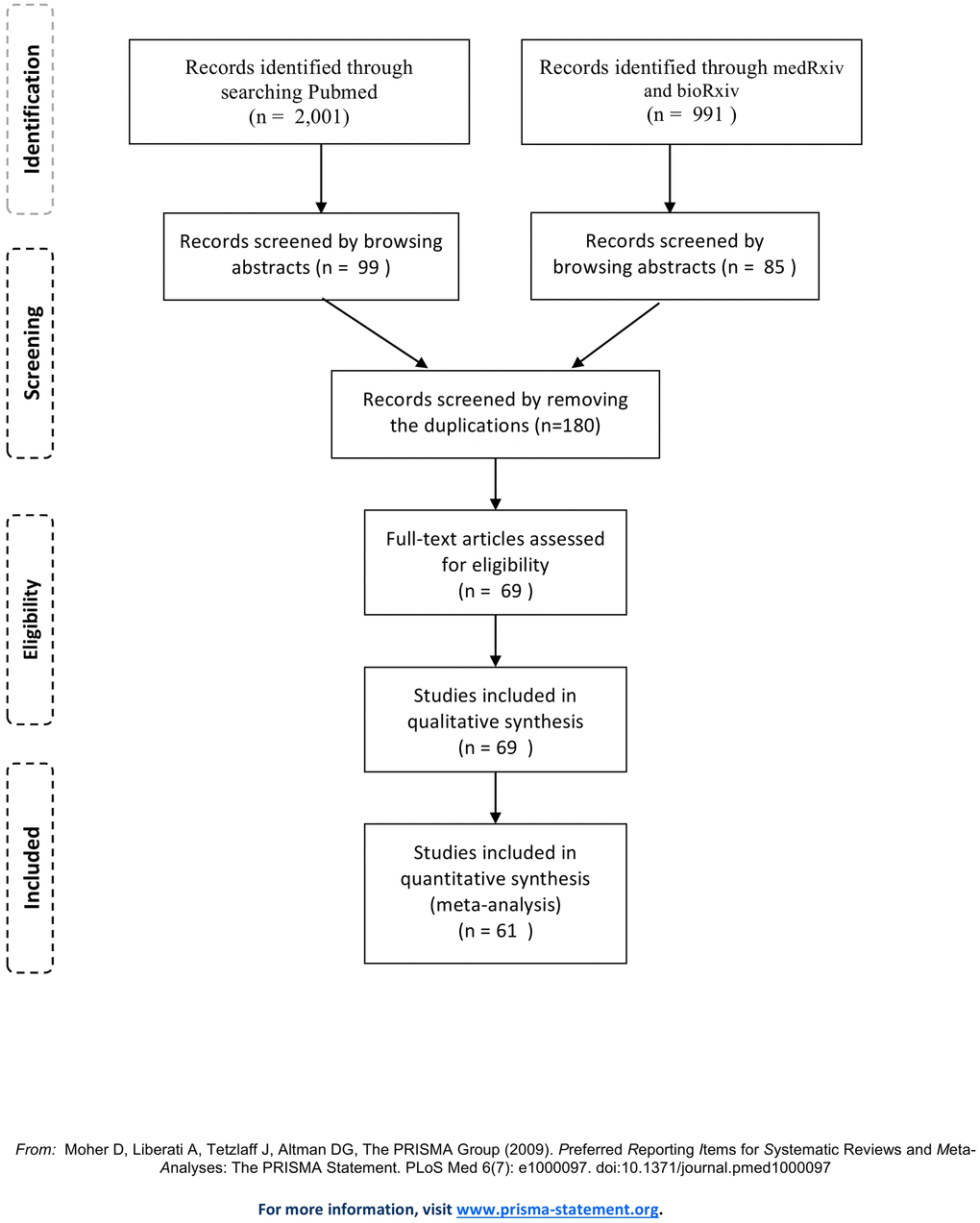
Figure 1. PRISMA flow diagram.
Quantitative data synthesis
The forest plots for all quantitative data synthesis of the epidemiological, comorbidity factors with severity and prognosis of COVID-19 were shown in supplementary materials (Supplementary Figures 1–120). Table 1 presents the quantitative results for the associations of the dichotomous epidemiological, comorbidity factors with severity of COVID-19. First, we found that the males had significant higher disease severity (RR: 1.20, 95% CI: 1.13-1.27, P <0.001, No. of cases: 8916). Besides, comorbidities, including any comorbidities, hypertension, diabetes, malignancy, cardiovascular disease, coronary heart disease, cerebrovascular disease, cardiovascular/cerebrovascular disease, chronic obstructive pulmonary disease (COPD), respiratory system disease, chronic kidney disease, hepatitis B infection, and digestive disease were significantly associated with the disease severity (all P <0.05). Of them, the top 3 effect sizes for the severity of COVID-19 were detected for COPD (RR: 4.20, 95% CI: 2.82-6.25, P<0.001), respiratory system disease (RR: 3.25, 95% CI: 2.48-4.27, P<0.001), and cerebrovascular disease (RR: 2.77, 95% CI: 1.70-4.52, P<0.001).
Table 1. Quantitative data synthesis for the associations of the epidemiological, comorbidity factors with severity of COVID-19.
| Variables | No of studies | Total cases | P heterogeneity | I2 (%) | RR (95% CIs) | P value | P Egger |
| Sex, male | 33 | 8916 | 0.078 | 27.2 | 1.20 (1.13-1.27) | <0.001 | 0.040 |
| Smoking | 11 | 5237 | <0.001 | 80.8 | 1.56 (0.95-2.57) | 0.082 | 0.956 |
| Current smoking | 2 | 2879 | 0.133 | 55.6 | 1.17 (0.92-1.50) | 0.198 | - |
| Ex-smoking | 2 | 2879 | 0.019 | 81.7 | 2.17 (0.61-7.70) | 0.232 | - |
| Drinking | 4 | 2274 | 0.067 | 58.0 | 0.83 (0.48-1.44) | 0.516 | 0.722 |
| Local residents of Wuhan | 4 | 1931 | <0.001 | 90.9 | 0.66 (0.32-1.36) | 0.256 | 0.441 |
| Exposure to Hubei Province | 10 | 3127 | <0.001 | 90.9 | 1.21 (0.88-1.65) | 0.240 | 0.115 |
| Contact with confirmed or suspect cases | 13 | 5007 | 0.041 | 45.8 | 0.98 (0.86-1.13) | 0.801 | 0.072 |
| Family cluster | 5 | 2578 | 0.857 | 0.0 | 0.94 (0.86-1.04) | 0.224 | 0.856 |
| Huanan seafood market exposure | 5 | 2342 | 0.001 | 79.9 | 1.79 (0.38-8.35) | 0.459 | 0.212 |
| Comorbidities | 16 | 6219 | <0.001 | 83.4 | 1.72 (1.44-2.06) | <0.001 | 0.710 |
| Hypertension | 23 | 7739 | <0.001 | 75.0 | 2.09 (1.74-2.52) | <0.001 | 0.154 |
| Diabetes | 23 | 7739 | 0.017 | 42.6 | 1.95 (1.60-2.36) | <0.001 | 0.272 |
| Malignancy | 14 | 5905 | 0.137 | 30.0 | 1.56 (1.11-2.21) | 0.011 | 0.644 |
| Cardiovascular disease | 18 | 6841 | 0.019 | 45.5 | 2.74 (2.03-3.70) | <0.001 | <0.001 |
| Coronary heart disease | 8 | 3899 | 0.087 | 43.7 | 2.03 (1.39-2.15) | <0.001 | 0.040 |
| Cerebrovascular disease | 12 | 5756 | 0.074 | 40.0 | 2.77 (1.70-4.52) | <0.001 | 0.595 |
| Cardiovascular/cerebrovascular disease | 6 | 3057 | <0.001 | 84.0 | 2.31 (1.31-4.08) | 0.004 | 0.502 |
| COPD | 14 | 6609 | 0.492 | 0.0 | 4.20 (2.82-6.25) | <0.001 | 0.580 |
| Respiratory system disease | 18 | 7522 | 0.661 | 0.0 | 3.25 (2.48-4.27) | <0.001 | 0.577 |
| Chronic kidney disease | 15 | 4861 | 0.173 | 25.5 | 2.27 (1.55-3.32) | <0.001 | 0.179 |
| Chronic liver disease | 11 | 3248 | 0.201 | 25.5 | 1.35 (0.89-2.05) | 0.165 | 0.782 |
| Hepatitis B infection | 3 | 1710 | 0.448 | 0.0 | 2.69 (1.32-5.51) | 0.007 | 0.735 |
| Lithiasis | 2 | 308 | 0.873 | 0.0 | 3.03 (0.73-12.58) | 0.127 | - |
| Autoimmune disease | 5 | 2202 | 0.727 | 0.0 | 2.52 (0.80-7.90) | 0.113 | 0.997 |
| Abnormal lipid metabolism | 4 | 2246 | 0.648 | 0.0 | 0.57 (0.26-1.25) | 0.162 | 0.080 |
| Digestive disease | 5 | 1013 | 0.492 | 0.0 | 1.80 (1.13-2.87) | 0.014 | 0.717 |
| Thyroid disease | 3 | 348 | 0.350 | 0.0 | 2.37 (0.66-8.50) | 0.186 | 0.387 |
| Tuberculosis | 2 | 592 | 0.473 | 0.0 | 2.74 (0.72-10.4) | 0.141 | - |
| Nervous system disease | 3 | 796 | 0.368 | 0.0% | 1.64 (0.68-3.93) | 0.270 | 0.160 |
| Endocrine system disease | 3 | 796 | <0.001 | 89.6 | 3.09 (0.70-13.64) | 0.136 | 0.622 |
We also explored the associations of the dichotomous epidemiological, comorbidity factors with prognosis of COVID-19 (Supplementary Table 2, and Table 2). The males had higher risk of developing the endpoints including death, ARDS, admission to ICU, invasive ventilation, and cardiac abnormality. Hypertension was found to be associated with all seven endpoints, cardiovascular disease and cerebrovascular disease with 6 (except for disease progression), respiratory system disease with 6 (except for Cardiac abnormality), COPD with 5 (except for ARDS and cardiac abnormality), diabetes with 5 (except for the composite endpoint, cardiac abnormality), malignancy with 2 (death, and admission to ICU), etc. Among them, chronic kidney disease contributed mostly for death (RR: 7.10, 95% CI: 3.14-16.02, P<0.001), COPD for admission to ICU (RR: 5.61, 95% CI: 2.68-11.76, P<0.001), the composite endpoint (RR: 8.52, 95% CI: 4.36-16.65, P<0.001), invasive ventilation (RR: 6.53, 95% CI: 2.70-15.84, P<0.001), and disease progression (RR: 7.48, 95% CI: 1.60-35.05, P =0.011), cerebrovascular disease for ARDS (RR: 3.15, 95% CI: 1.23-8.04, P =0.016), coronary heart disease for cardiac abnormality (RR: 5.37, 95% CI: 1.74-16.54, P =0.003). Besides, the associations of continuous age with severity and prognosis of COVID-19 were presented in Table 3. Older age was found to be significantly associated with the disease severity and six endpoints (all P value <0.001, except a marginal association for disease progression). The biggest standard mean difference (SMD) was detected for death (SMD: 1.06, 95% CI: 0.85-1.26, P<0.001). However, we didn’t find any statistically significant associations for epidemiological factors, including drinking, local residents of Wuhan, exposure to Hubei Province, contact with confirmed or suspect cases, family cluster, and Huanan seafood market exposure. Sensitivity analyses by changing the pooling model and statistical variables, or using one-at-a-time method, were performed to assess the stability of the results. However, we found the results were not materially changed (data not shown). Further, we applied the Egger test to evaluated the potential publication bias, and very litter evidence (among all 120 associations, only 6 presented the existence of possible publication bias) was detected (Tables 1–3 and Supplementary Table 2).
Table 2. Quantitative data synthesis for the associations of the epidemiological, comorbidity factors with prognosis of COVID-19 (P value<0.05).
| Variables | No of studies | Total cases | P heterogeneity | I2 (%) | RR (95% CIs) | P value | P Egger |
| Death | | | | | | | |
| Sex, male | 10 | 4214 | 0.443 | 0.0 | 1.23 (1.14-1.33) | <0.001 | 0.276 |
| Comorbidities | 8 | 4499 | <0.001 | 88.7 | 1.68 (1.32-2.13) | <0.001 | 0.248 |
| Hypertension | 11 | 4860 | <0.001 | 84.4 | 1.74 (1.31-2.30) | <0.001 | 0.418 |
| Diabetes | 10 | 4748 | 0.001 | 67.1 | 1.75 (1.27-2.41) | 0.001 | 0.057 |
| Malignancy | 6 | 3978 | 0.262 | 22.8 | 3.09 (1.59-6.00) | 0.001 | 0.006 |
| Cardiovascular disease | 11 | 4860 | <0.001 | 75.9 | 2.67 (1.60-4.43) | <0.001 | 0.654 |
| Coronary heart disease | 5 | 2452 | <0.001 | 87.7 | 3.16 (1.45-6.91) | 0.004 | 0.435 |
| Cerebrovascular disease | 6 | 3771 | 0.457 | 0.0 | 4.61 (2.51-8.47) | <0.001 | 0.766 |
| COPD | 4 | 3677 | 0.279 | 22.0 | 5.31 (2.63-10.71) | <0.001 | 0.107 |
| Respiratory system disease | 7 | 4472 | 0.185 | 31.8 | 3.22 (2.12-4.90) | <0.001 | 0.761 |
| Chronic kidney disease | 5 | 2219 | 0.477 | 0.0 | 7.10 (3.14-16.02) | <0.001 | 0.772 |
| Admission to ICU | | | | | | | |
| Sex, male | 5 | 2224 | 0.011 | 69.6 | 1.29 (1.13-1.47) | <0.001 | 0.651 |
| Comorbidities | 5 | 3747 | 0.038 | 60.5 | 1.82 (1.45-2.29) | <0.001 | 0.646 |
| Hypertension | 5 | 3747 | 0.601 | 0.0 | 2.31 (1.97-2.70) | <0.001 | 0.312 |
| Diabetes | 5 | 3747 | 0.084 | 51.4 | 1.88 (1.10-3.23) | 0.021 | 0.457 |
| Malignancy | 5 | 3747 | 0.427 | 0.0 | 2.52 (1.38-5.59) | 0.003 | 0.158 |
| Cardiovascular disease | 5 | 3747 | 0.511 | 0.0 | 2.74 (1.92-3.92) | <0.001 | 0.692 |
| Cerebrovascular disease | 3 | 3508 | 0.349 | 4.9 | 5.12 (2.86-9.17) | <0.001 | 0.273 |
| COPD | 4 | 3549 | 0.800 | 0.0 | 5.61 (2.68-11.76) | <0.001 | 0.740 |
| Respiratory system disease | 4 | 3549 | 0.613 | 0.0 | 4.66 (2.59-8.40) | <0.001 | 0.637 |
| Composite endpoint | | | | | | | |
| Smoking | 2 | 2879 | 0.604 | 0.0 | 2.67 (1.91-3.73) | <0.001 | - |
| Comorbidities | 2 | 3370 | <0.001 | 95.3 | 1.96 (1.06-3.60) | 0.031 | - |
| Hypertension | 2 | 3370 | 0.011 | 84.5 | 2.20 (1.44-3.36) | <0.001 | - |
| Cardiovascular disease | 2 | 3370 | 0.927 | 0.0 | 3.09 (2.09-4.57) | <0.001 | - |
| Coronary heart disease | 2 | 3370 | 0.473 | 0.0 | 3.36 (2.15-5.25) | <0.001 | - |
| Cerebrovascular disease | 2 | 3370 | 0.225 | 32.0 | 4.10 (2.34-7.18) | <0.001 | - |
| COPD | 2 | 3370 | 0.185 | 43.0 | 8.52 (4.36-16.65) | <0.001 | - |
| Respiratory system disease | 2 | 3370 | 0.185 | 43.0 | 8.52 (4.36-16.65) | <0.001 | - |
| ARDS | | | | | | | |
| Sex, male | 3 | 2090 | 0.464 | 0.0 | 1.15 (1.01-1.30) | 0.033 | 0.353 |
| Hypertension | 3 | 2090 | 0.377 | 0.0 | 1.90 (1.57-2.30) | <0.001 | 0.520 |
| Diabetes | 3 | 2090 | 0.068 | 62.9 | 3.07 (1.28-7.36) | 0.012 | 0.066 |
| Cardiovascular disease | 3 | 2090 | 0.244 | 29.2 | 2.26 (1.43-3.58) | <0.001 | 0.422 |
| Cerebrovascular disease | 2 | 1889 | 0.152 | 51.2 | 3.15 (1.23-8.04) | 0.016 | - |
| Respiratory system disease | 2 | 1889 | 0.303 | 5.6 | 2.44 (1.20-4.97) | 0.014 | - |
| Invasive ventilation | | | | | | | |
| Sex, male | 2 | 1825 | 0.403 | 0.0 | 1.35 (1.11-1.64) | 0.002 | - |
| Family cluster | 2 | 1825 | 0.646 | 0.0 | 1.58 (1.13-2.14) | 0.006 | - |
| Comorbidities | 3 | 3415 | 0.005 | 81.2 | 1.83 (1.19-2.79) | 0.006 | 0.569 |
| Hypertension | 3 | 3415 | 0.131 | 50.9 | 2.35 (1.92-2.89) | <0.001 | 0.366 |
| Diabetes | 3 | 3415 | 0.131 | 50.8 | 1.85 (1.24-2.76) | 0.003 | 0.021 |
| Cardiovascular disease | 3 | 3415 | 0.844 | 0.0 | 2.90 (1.63-5.15) | <0.001 | 0.618 |
| Cerebrovascular disease | 2 | 3370 | 0.602 | 0.0 | 3.98 (1.77-8.93) | 0.001 | - |
| COPD | 2 | 3370 | 0.383 | 0.0 | 6.53 (2.70-15.84) | <0.001 | - |
| Respiratory system disease | 3 | 3415 | 0.260 | 25.7 | 4.34 (2.04-9.26) | <0.001 | 0.567 |
| Cardiac abnormality | | | | | | | |
| Sex, male | 4 | 439 | 0.211 | 33.6 | 1.33 (1.02-1.72) | 0.036 | 0.624 |
| Hypertension | 4 | 439 | 0.947 | 0.0 | 2.97 (1.65-5.34) | <0.001 | 0.610 |
| Cardiovascular disease | 4 | 439 | 0.915 | 0.0 | 4.90 (1.82-13.21) | 0.002 | 0.177 |
| Coronary heart disease | 3 | 386 | 0.819 | 0.0 | 5.37 (1.74-16.54) | 0.003 | 0.408 |
| Disease progression | | | | | | | |
| Hypertension | 2 | 219 | 0.547 | 0.0 | 2.90 (1.45-5.81) | 0.003 | - |
| Diabetes | 2 | 219 | 0.746 | 0.0 | 3.30 (1.08-10.07) | 0.036 | - |
| COPD | 2 | 219 | 0.848 | 0.0 | 7.48 (1.60-35.05) | 0.011 | - |
| Respiratory system disease | 2 | 219 | 0.848 | 0.0 | 7.48 (1.60-35.05) | 0.011 | - |
Table 3. Quantitative data synthesis for the associations of age with severity and prognosis of COVID-19.
| Variables | No of studies | Total cases | P heterogeneity | I2 (%) | SMD (95% CIs) | P value | P Egger |
| Severity | 32 | 8140 | <0.001 | 92.4 | 0.73 (0.53-0.94) | <0.001 | 0.331 |
| Death | 9 | 3725 | 0.005 | 63.9 | 1.06 (0.85-1.26) | <0.001 | 0.610 |
| Admission to ICU | 5 | 2224 | 0.189 | 34.9 | 0.78 (0.60-0.96) | <0.001 | 0.538 |
| Composite endpoint | 2 | 2879 | 0.055 | 72.9 | 0.88 (0.56-1.21) | <0.001 | - |
| ARDS | 3 | 2090 | 0.939 | 0 | 0.83 (0.67-0.99) | <0.001 | 0.882 |
| Invasive ventilation | 2 | 1825 | 0.493 | 0.0 | 0.84 (0.54-1.14) | <0.001 | - |
| Cardiac abnormality | 4 | 439 | 0.041 | 63.6 | 0.92 (0.44-1.41) | <0.001 | 0.885 |
| Disease progression | 2 | 219 | <0.001 | 95.4 | 2.37 (0.00-4.74) | 0.050 | - |