Prediction of pregnancy outcome in fresh in vitro fertilization/intracytoplasmic sperm injection treatment in patients with poor ovarian reserve
Abstract
We retrospectively analyzed the clinical data from 39,185 cycles who undergoing in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI) in the First People's Hospital of Shangqiu, these poor ovarian reserve patients were further categorized into the "unexpected" group (n=3337) and the "expected" group (n=2667) based on POSEIDON classification. In "expected" group, logistic regression analysis showed that female age (OR 0.920; 95% C.I 0.902~0.939; P < 0.001), treatment cycles (OR 0.693; 95% C.I 0.560~0.859; P = 0.001), duration of Gn administered (OR 1.077; 95% C.I 1.027~1.129; P = 0.002) and transferable embryos (OR 1.377; 95% C.I 1.319~1.437; P < 0.001) is independent predictive factors of live birth. In "expected" group, logistic regression analysis showed that female age (OR 0.874; 95% C.I 0.848~0.900; P < 0.001), AFC (OR 1.285; 95% C.I 1.131~1.461; P < 0.001), total dosage of Gn administered (OR 1.001; 95% C.I 1.000~1.002; P < 0.001), duration of Gn administered (OR 0.784; 95% C.I 0.639~0.961; P = 0.019), MII number (OR 0.841; 95% C.I 0.717~0.986; P = 0.032) and transferable embryos (OR 2.057; 95% C.I 1.762~2.400; P < 0.001) is independent predictive factors of live birth. We also established a smooth curve fit to predict the probability of live birth among the POSEIDON "unexpected" and "expected" group. These independent predictive factors on the pregnancy outcome of IVF/ICSI and the successful establishment of smooth curve fit can provide valuable reference for treats poor ovarian reserve patients in clinical work.
Introduction
How to accurately predict pregnancy outcome in patients with poor ovarian response (POR) remains one of the most elusive medical breakthroughs in humans following assisted reproduction. Despite numerous research efforts, there is no consensus on factors that accurately predict the outcome of in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI) [1, 2]. This has been in part occasioned by poorly understood diagnosis and mechanisms underlying POR development [3, 4], which has frustrated diagnosis and management of infertility among couples. Overall, independent factors that predict pregnancy outcome in POR patients remain to be validated [5].
The new POSEIDON stratification guidelines which classify patients with infertility condition in to "expected" or "unexpected" groups with regard to successful live birth have been embraced by reproductive endocrinologists worldwide. They provide a more nuanced picture for the management of POR individuals in need of reproduction assistance [6, 7]. The POSEIDON concept provides pragmatic clinical recommendations for POR individuals [8]. Live births were based on the number of oocytes needed to obtain one euploid embryo for transfer in each patient [9]. Compared with the Bologna criteria, POSEIDON guides on the diagnosis and management of POR. However, on few researches have been conducted to unravel female-related parameters and independent factors that predict pregnancy outcomes among POR patients, particularly those in POSEIDON clusters. Over the past three decades, several experimental studies have evaluated independent predictive factors for pregnancy outcome following IVF / ICSI in fertile people [10]. Most of the known predictive factors have become part of the routine diagnostic procedure for infertile patients who undergo assisted reproduction. However, comprehensive data specific for POR individuals is either controversial or lacking [11]. The current global aim is to accurately predict the probability of successful pregnancy or live birth in infertile POR patients [12, 13]. This underscores the need to evaluate factors influencing the probability of live birth in POR patients, particularly those in POSEIDON clusters.
Evidence-based medicine has progressively transformed in to the standard approach for numerous diagnosis and treatment of several health complications [14]. Accordingly, we retrospectively analyzed clinical data of 39,185 individuals who underwent IVF/ICSI at the First People's Hospital of Shangqiu, center for reproductive health. We aimed to uncover independent factors for predicting pregnancy outcome among POSEIDON "unexpected" and "expected" group. Findings of this study can improve the management of infertile individual desiring to sire children.
Results
Patient characteristics
POR patients were divided in to "unexpected" group (n=3337) and "expected" group (n=2667). Live birth was observed in 1134 (33.98%) women in the "unexpected" group. The rest of the 2203 (66.02%) women didn't get a live birth. In the "expected" group, 220 (8.25%) women delivered live babies, whereas 2447 (91.75%) of them didn't get a live birth.
Baseline characteristics and independent risk factors for the live birth in the "unexpected" group
Baseline characteristics of patients in the "unexpected" group and likely predictive factors for successful pregnancies are shown in Table 1. Univariate logistic regression analysis revealed that the female age, years of infertility, BMI, basal LH, AMH, AFC, treatment cycles, Gn dosage, duration of Gn administration, number transferable embryos significantly influenced the prospect of live birth. However, multivariate logistic regression analysis showed that the female age (OR 0.920; 95% C.I 0.902~0.939; P < 0.001), number of treatment cycles (OR 0.693; 95% C.I 0.560~0.859; P = 0.001), duration of Gn administration (OR 1.077; 95% C.I 1.027~1.129; P = 0.002) and number transferable embryos (OR 1.377; 95% C.I 1.319~1.437; P < 0.001) were the only independent predictive factors for live birth. Smooth curve fitting showed that female age and treatment cycles increased the risk of unsuccessful births, whereas Gn administration and transferable embryos lowered the risk of unsuccessful births. However, there were no simple linear relationships, threshold effects and nonlinear association were found between female age, number of treatment cycles as well as duration of Gn administration and live birth (Figure 1).
Table 1. Baseline characteristics of patients with LB and non-LB and independent risk factors for the pregnancy results in the "unexpected" group.
| Factors | Baseline characteristics | Unadjusted | Adjusted |
| LB (1134) | non-LB (2203) | OR | 95% C.I | P | OR | 95% C.I | P |
| Age (years) | 30.9±4.3 | 33.5±5.6 | 0.904 | 0.891~0.918 | 0.000 | 0.920 | 0.902~0.939 | 0.000 |
| Infertility years | 4.1±2.9 | 4.7±3.7 | 0.939 | 0.919~0.961 | 0.000 | 0.979 | 0.954~1.006 | 0.124 |
| BMI (Kg/M2) | 22.7±3.2 | 23.0±5.0 | 0.973 | 0.951~0.994 | 0.014 | 0.989 | 0.965~1.013 | 0.361 |
| Basal FSH (IU/L) | 7.0±2.1 | 7.0±2.0 | 1.013 | 0.979~1.048 | 0.469 | / | / | / |
| Basal LH (IU/L) | 5.7±3.5 | 5.4±3.3 | 1.026 | 1.005~1.048 | 0.015 | 0.997 | 0.972~1.022 | 0.791 |
| Basal E2 (ng/L) | 40.4±27.9 | 41.1±29.2 | 0.999 | 0.997~1.002 | 0.464 | / | / | / |
| Basal P (μg/L) | 0.6±0.7 | 0.6±0.7 | 1.042 | 0.940~1.155 | 0.437 | / | / | / |
| AMH (ng/mL) | 3.4±2.8 | 3.0±2.2 | 1.065 | 1.035~1.095 | 0.000 | 0.992 | 0.950~1.037 | 0.734 |
| AFC(n) | 13.7±5.8 | 12.4±5.7 | 1.037 | 1.025~1.050 | 0.000 | 0.998 | 0.979~1.017 | 0.825 |
| No. of treatment cycles | 2.1±0.3 | 2.2±0.7 | 0.570 | 0.470~0.692 | 0.000 | 0.693 | 0.560~0.859 | 0.001 |
| Total dosage of Gn used | 2661.9±994.1 | 2833.6±956.5 | 1.000 | 1.000~1.000 | 0.000 | 1.000 | 1.000~1.000 | 0.348 |
| Duration of Gn used | 12.7±2.5 | 12.3±2.6 | 1.067 | 1.038~1.098 | 0.000 | 1.077 | 1.027~1.129 | 0.002 |
| Oocyte number | 7.8±2.7 | 7.9±4.1 | 0.990 | 0.971~1.010 | 0.320 | / | / | / |
| MII number | 6.3±2.6 | 6.2±3.7 | 1.016 | 0.995~1.038 | 0.137 | / | / | / |
| Transferable embryos | 3.5±1.7 | 2.4±1.9 | 1.382 | 1.326~1.441 | 0.000 | 1.377 | 1.319~1.437 | 0.000 |
| Data are shown as means ± standard deviation. BMI, body mass index; FSH, follicular-stimulating hormone; LH, luteinizing hormone; E2, estradiol; P, progesterone; AMH, anti-Müllerian hormone; AFC, antral follicle counting; LB, live birth; Gn, Gonadotropin. |
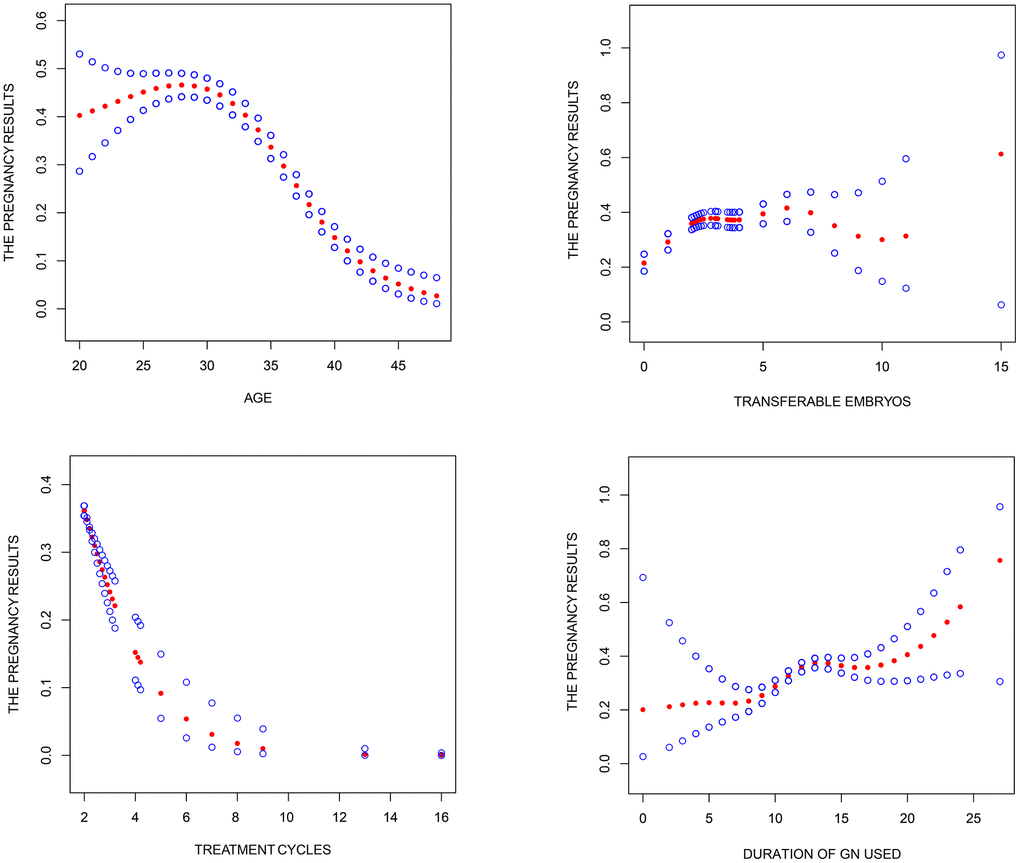
Figure 1. Association between pregnancy outcome and female age, treatment cycles, duration of Gn used and transferable embryos in "unexpected" group. A threshold, nonlinear association between pregnancy outcome and these independent predictive factors was found (P<0.05) in a generalized additive model (GAM). Solid rad line represents the smooth curve fit between variables. Blue bands represent the 95% of confidence interval from the fit. Pregnancy outcome was defined as live birth rate; Gn.
Baseline characteristics and independent risk factors for the live birth in the "expected" group
The baseline characteristics of patients in the "expected" group are shown in Table 2. Univariate logistic regression analysis showed that the female age, years of infertility, basal FSH, basal LH, basal E2, AMH, AFC, number of treatment cycles, total Gn dosage, duration of Gn administration, number of oocytes, MII number and number of transferable embryos significantly influenced the probability of live birth. However, multivariate logistic regression analysis showed that the female age (OR 0.874; 95% C.I 0.848~0.900; P < 0.001), AFC (OR 1.285; 95% C.I 1.131~1.461; P < 0.001), total dosage of Gn administered (OR 1.001; 95% C.I 1.000~1.002; P < 0.001), duration of Gn administration (OR 0.784; 95% C.I 0.639~0.961; P = 0.019), MII number (OR 0.841; 95% C.I 0.717~0.986; P = 0.032) and number of transferable embryos (OR 2.057; 95% C.I 1.762~2.400; P < 0.001) were independent predictive factors for live birth. Smooth curve fitting showed that female age, duration of Gn administered and MII increased the risk of live birth, whereas having antral follicles, total Gn administration and transferable embryos increased the chance of live birth. However, smooth curve fitting showed no substantial nonlinear association between female age, total dosage of Gn administered, duration of Gn administered, MII number as well as transferable embryos and live birth (Figure 2).
Table 2. Baseline characteristics of patients with LB and non-LB and independent risk factors for the pregnancy results in the "expected" group.
| Factors | Baseline characteristics | Unadjusted | Adjusted |
| LB (220) | non-LB (2447) | OR | 95% C.I | P | OR | 95% C.I | P |
| Age (years) | 34.3±5.0 | 39.2±5.5 | 0.869 | 0.849~0.890 | 0.000 | 0.874 | 0.848~0.900 | 0.000 |
| Infertility years | 4.5±3.3 | 5.3±4.7 | 0.959 | 0.927~0.992 | 0.014 | 0.986 | 0.946~1.029 | 0.528 |
| BMI (Kg/M2) | 23.2±3.0 | 23.4±4.3 | 0.985 | 0.941~1.032 | 0.522 | / | / | / |
| Basal FSH (IU/L) | 9.8±5.2 | 12.1±6.7 | 0.933 | 0.908~0.960 | 0.000 | 0.985 | 0.946~1.026 | 0.459 |
| Basal LH (IU/L) | 4.7±2.4 | 5.9±4. | 0.906 | 0.862~0.953 | 0.000 | 0.982 | 0.922~1.047 | 0.586 |
| Basal E2 (ng/L) | 48.6±44.0 | 58.2±62.5 | 0.997 | 0.994~1.000 | 0.027 | 0.999 | 0.995~1.003 | 0.719 |
| Basal P (μg/L) | 0.5±0.3 | 0.5±0.5 | 0.731 | 0.499~1.069 | 0.106 | / | / | / |
| AMH (ng/mL) | 0.6±0.3 | 0.4±0.3 | 8.110 | 5.255~12.516 | 0.000 | 1.183 | 0.633~2.210 | 0.599 |
| AFC(n) | 2.8±1.3 | 2.2±1.3 | 1.474 | 1.310~1.657 | 0.000 | 1.285 | 1.131~1.461 | 0.000 |
| No. of treatment cycles | 1.5±1.0 | 2.2±1.7 | 0.612 | 0.523~0.717 | 0.000 | 0.912 | 0.773~1.075 | 0.271 |
| Total dosage of Gn used | 3761.8±879.3 | 2725.2±1400.2 | 1.001 | 1.000~1.001 | 0.000 | 1.001 | 1.000~1.002 | 0.001 |
| Duration of Gn used | 12.8±2.9 | 10.0±4.1 | 1.182 | 1.141~1.224 | 0.000 | 0.784 | 0.639~0.961 | 0.019 |
| Oocyte number | 5.5±3.3 | 2.5±2.4 | 1.342 | 1.286~1.401 | 0.000 | 1.084 | 0.957~1.228 | 0.203 |
| MII number | 4.5±2.8 | 2.0±2.1 | 1.401 | 1.331~1.474 | 0.000 | 0.841 | 0.717~0.986 | 0.032 |
| Transferable embryos | 2.7±1.4 | 0.9±1.2 | 2.138 | 1.946~2.349 | 0.000 | 2.057 | 1.762~2.400 | 0.000 |
| Data are shown as means ± standard deviation. BMI, body mass index; FSH, follicular-stimulating hormone; LH, luteinizing hormone; E2, estradiol; P, progesterone; AMH, anti-Müllerian hormone; AFC, antral follicle counting; LB, live birth; Gn, Gonadotropin. |
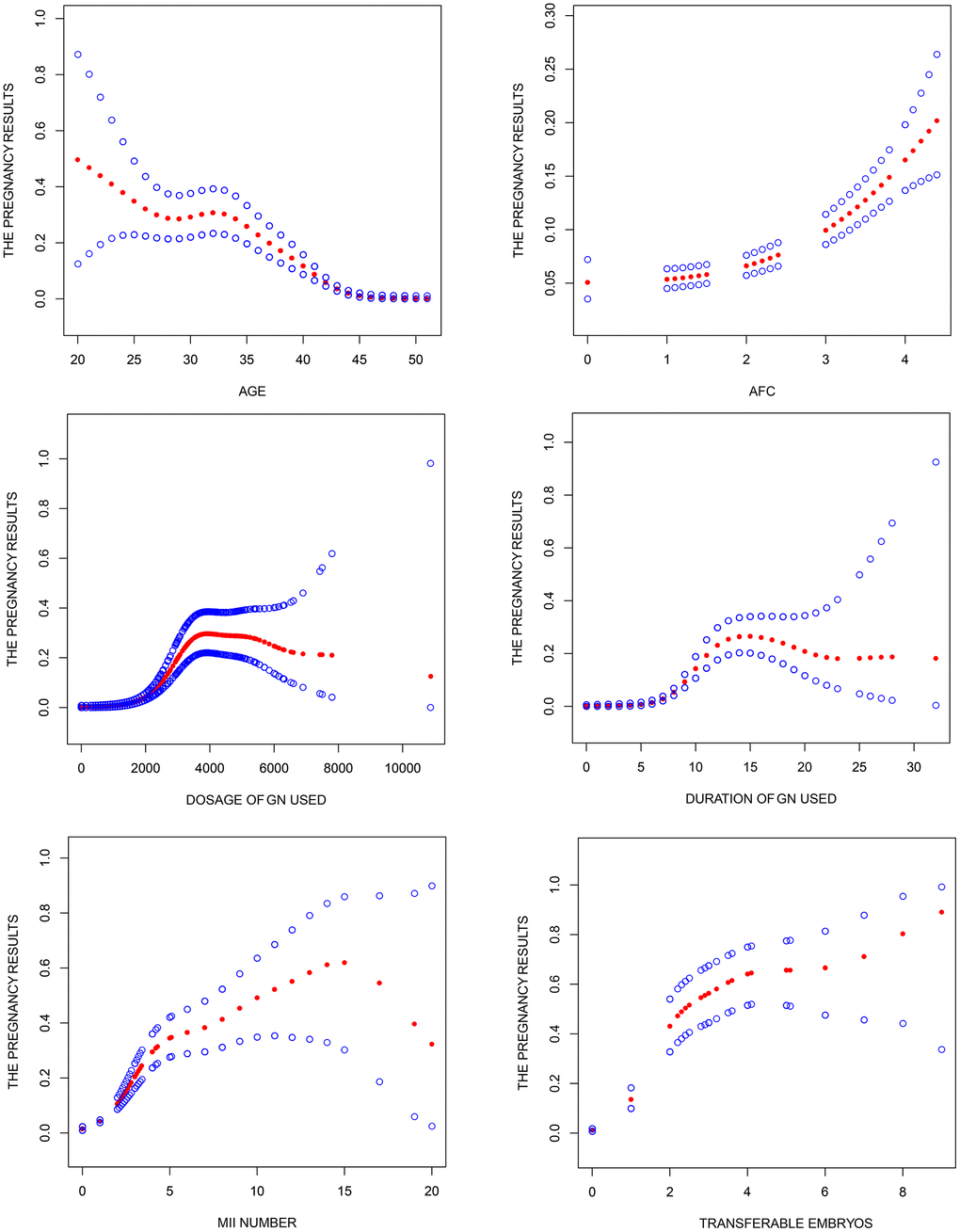
Figure 2. Association between pregnancy outcome and female age, AFC, total dosage of Gn used, duration of Gn used, MII number and transferable embryos in "expected" group. A threshold, nonlinear association between pregnancy outcome and these independent predictive factors was found (P<0.05) in a generalized additive model (GAM). Solid rad line represents the smooth curve fit between variables. Blue bands represent the 95% of confidence interval from the fit. Pregnancy outcome was defined as live birth rate, Gn, Gonadotropin; AFC, antral follicle counting.
Discussion
Herein, we analyzed factors that potentially predicts pregnancy outcome after IVF/ICIS among POSEIDON "unexpected" and "expected" groups in POR patients. Assisted reproductive technologies (ART) have significantly improved pregnancy outcomes in POR patients. However, intervening factors for pregnancy outcome in these group of individuals remain uncertain [15]. Also, how POR individuals respond to ART remain unclear. Only few researches have evaluated female-related parameters that independently predict pregnancy outcome in POR patients, particularly those in POSEIDON expected and unexpected clusters. Accordingly, we aimed to bring this to light.
Studies have shown that age of female is the most important factor affecting female fecundity and oocyte quality, all which directly affects pregnancy outcome whether in "unexpected" and "expected" group. Herein, we found a strong relationship between female age and the likelihood of live birth, consistent with previous findings. Particularly age and the propensity of live birth display an inverse relationship. Ovarian function decline with age, which positively correlates with decrease in the number and quality of oocytes [16]. Fewer and weak oocytes lowers the chance of successful pregnancy following IVF/ICSI [17]. Also, monochromatic abnormalities in oocytes and aneuploidy in preimplantation embryos are more common in older women, and are the main causes of miscarriage and lower live birth rates in aged women [16]. Overwhelming evidence shows that reproduction, age-related changes in women such as quantity and quality of oocytes begin at 35. Accordingly, ART live birth rates begin to decline at this age [1, 18]. On the other hand, there is no consensus on the role of FSH and AMH in pregnancy outcome [19, 20]. Herein, we found FSH and AMH levels had no significant effect on pregnancy outcome in both "unexpected" and "expected" POSEIDON clusters. Maseelall et al. also found that AFC is stronger predictor of ovarian response and pregnancy outcome than FSH [13]. and the AFC has been proved to be the best predictor of clinical practice [21, 22]. Studies show that production of more than 6 mature oocytes increases the probability of successful pregnancy by 61.5% [23], consistent with our findings. However, given the selection bias in retrospective studies, randomized controlled trials are needed to validate the relationship between them.
Multivariate logistic regression analysis revealed that age of female, treatment cycles, duration of Gn administered and transferable embryos were independent predictive factors of live birth in the "unexpected" POSEIDON group. our study show that the chances of achieving a successful pregnancy outcome decreases with increasing female age and increasing treatment cycles, however, there is a positive correlation association between the chance of pregnancy and duration of Gn administered and transferable embryos. It is worth emphasizing that there are no simple linear relationship between them observed through smooth curve fit, threshold effects and nonlinear association were found between female age, treatment cycles, duration of Gn administered and live birth, through the integration of large sample data and the smooth curve fit, we can predict the live birth rate more accurately and successfully. And we can found female age maybe in 20 to 30 years had the highest live birth among the "unexpected" group, Meanwhile, the probability of females older than 45 years in the "unexpected" POSEIDON group getting pregnant was generally zero. Also, we found a strong relationship between live birth rate and number of treatment cycles, duration of Gn administration and the number of transferable embryos in POR patients.
Age of female, AFC level, total dosage of Gn administered, duration of Gn administration, number of MII and transferable embryos were independent predictors of live birth in the "expected" group. We found age of female, duration of Gn administration and MII number influences the probability of live birth, whereas AFC, total dosage of Gn administered and number of transferable embryos protective factor for live birth rate. Smooth curve fit revealed that these independent predictors can accurately predict the probability of live birth in POR patients, thus useful in clinical management of these group of individuals. Even so, many factors and functioning of many systems continuous change during pregnancy, coupled by numerous confounding factors. Also, retrospective trials suffer substantial selection bias issues, which impacts on the outcome, we will conduct RCT to confirm this hypothesis in the future.
Overall, the POSEIDON classification system of individuals with infertility complication in to "expected" or "unexpected" groups is useful in clinical diagnosis and management of these patients [24, 25]. This enhances probability of live birth after IVF/ICSI.
Materials and Methods
Clinical data for 39,185 women undergoing IVF/ICSI at reproductive medical center of the First People's Hospital of Shangqiu were enrolled for this study. Eligible participants were categorized into "unexpected" (n=3337) or "expected" group (n=2667) based on POSEIDON criteria. According to POSEIDON guidelines, patients with antral follicle count (AFC) ≥ 5, anti-Mulller hormones(AMH) ≥ 1.2 ng/ml and ≤ 9 oocytes retrieved in the first simulation cycle are (not expected) to have successful deliveries, whereas those with AFC < 5, AMH < 1.2ng/ml are (expected/ not expected) to have successful pregnancies [26, 27].
The patients either received prolonged GnRH agonist or GnRH antagonist treatment, short GnRH agonist treatment or natural cycle of IVF/ICSI followed by embryo transfer in the same cycle. The starting gonadotropin dose was based on the AFC, age of female patient, body mass index (BMI) and previous history of ovarian response to stimulation. The doses were adjusted progressively according to patient`s response. When dominant follicles measuring > 16mm reached 60% or the mean follicle diameter reached 20 mm, (ovulation) triggering was performed using 250ug r-hCG (Merck Serono) in combination with 2000IU u-HCG (Livzon Pharmaceuticals). Oocyte were retrieved 37 hours after triggering using transvaginal ultrasound [28]. Successful pregnancy outcome was defined as at least one baby born alive, or a live fetus born after 28 weeks of gestation [29].
Various parameters and likely intervening factors for successful birth were compared between groups. The data used in this study was downloaded from the Clinical Reproductive Medicine Management System/Electronic Medical Record Cohort Database (CCRM/EMRCD) of the First People's Hospital of Shangqiu, Reproductive Medical Center. The patients had attended the hospital between January 2013 and December 2018. The protocol for this study was approved by the Ethics Committee of Reproductive Medicine Centre of the First People's Hospital of Shangqiu, China. Approved consents were not necessary. The research was performed in accordance with the First People's Hospital of Shangqiu guidelines and regulations.
Statistical analysis
Data was analyzed using R software, V. 3.2.3, EmpowerStats (http://www.empowerstats.com) and SPSS V. 19.0 (IBM, Armonk, NY, USA). Continuous variables were expressed as means ± standard deviation. Differences between groups were compared using Student’s t test or the Wilcoxon rank sum test. The relationship between various factors such as age of the female, years of infertility, BMI, AMH, AFC, number of transferable embryos, treatment cycles, Gn dosage, Gn duration, number of Oocytes, number of MII and number of transferable embryos among others, and pregnancy outcome was analyzed using univariate and multivariate logistic regression analyses. P < 0.05 was considered statistically significant. P-values were adjusted based on the Holm-Bonferroni method to control for Type I error.
Author Contributions
F. L. designed, conducted and supervised the general study. F.L., Y.C., F.X.M. responded for the patients selection and classification. A.Q.N, Y.L.Z reviewed and classified laboratory data for the patients. F.L. and Y.C. reviewed and F.L drafted and composed the manuscript. All authors reviewed this manuscript.
Acknowledgments
The authors thank for the women who participated in this study and all the physicians and nurses at the Reproductive Medicine Centre, the First People's Hospital of Shangqiu, China, for their support in collecting the data.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Funding
This work was supported by the Key Science and Technology Foundation of Henan Province (212102310049), the National Natural Science Foundation of China (81771534) and the Medical Science and Technology Co-construction Project of Henan Province (LHGJ20200933).
Editorial Note
&
This corresponding author has a verified history of publications using a personal email address for correspondence
References
-
1.
Scheffer JB, Scheffer BB, de Carvalho RF, Rodrigues J, Grynberg M, Mendez Lozano DH. Age as A Predictor of Embryo Quality Regardless of The Quantitative Ovarian Response. Int J Fertil Steril. 2017; 11:40–46. https://doi.org/10.22074/ijfs.2016.4579 [PubMed]
-
2.
Lamazou F, Genro V, Fuchs F, Grynberg M, Gallot V, Achour-Frydman N, Fanchin R, Frydman R. [Serum AMH level is not a predictive value for IVF in modified natural cycle: analysis of 342 cycles]. J Gynecol Obstet Biol Reprod (Paris). 2011; 40:205–10. https://doi.org/10.1016/j.jgyn.2011.02.002 [PubMed]
-
3.
Papathanasiou A, Searle BJ, King NM, Bhattacharya S. Trends in ‘poor responder’ research: lessons learned from RCTs in assisted conception. Hum Reprod Update. 2016; 22:306–19. https://doi.org/10.1093/humupd/dmw001 [PubMed]
-
4.
Patrizio P, Vaiarelli A, Levi Setti PE, Tobler KJ, Shoham G, Leong M, Shoham Z. How to define, diagnose and treat poor responders? Responses from a worldwide survey of IVF clinics. Reprod Biomed Online. 2015; 30:581–92. https://doi.org/10.1016/j.rbmo.2015.03.002 [PubMed]
-
5.
Broekmans FJ, Kwee J, Hendriks DJ, Mol BW, Lambalk CB. A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update. 2006; 12:685–718. https://doi.org/10.1093/humupd/dml034 [PubMed]
-
6.
Grynberg M, Labrosse J. Understanding Follicular Output Rate (FORT) and its Implications for POSEIDON Criteria. Front Endocrinol (Lausanne). 2019; 10:246. https://doi.org/10.3389/fendo.2019.00246 [PubMed]
-
7.
Esteves SC, Alviggi C, Humaidan P, Fischer R, Andersen CY, Conforti A, Bühler K, Sunkara SK, Polyzos NP, Galliano D, Grynberg M, Yarali H, Özbek IY, et al. The POSEIDON Criteria and Its Measure of Success Through the Eyes of Clinicians and Embryologists. Front Endocrinol (Lausanne). 2019; 10:814. https://doi.org/10.3389/fendo.2019.00814 [PubMed]
-
8.
Haahr T, Dosouto C, Alviggi C, Esteves SC, Humaidan P. Management Strategies for POSEIDON Groups 3 and 4. Front Endocrinol (Lausanne). 2019; 10:614. https://doi.org/10.3389/fendo.2019.00614 [PubMed]
-
9.
Alviggi C, Andersen CY, Buehler K, Conforti A, De Placido G, Esteves SC, Fischer R, Galliano D, Polyzos NP, Sunkara SK, Ubaldi FM, Humaidan P, and Poseidon Group (Patient-Oriented Strategies Encompassing IndividualizeD Oocyte Number). A new more detailed stratification of low responders to ovarian stimulation: from a poor ovarian response to a low prognosis concept. Fertil Steril. 2016; 105:1452–53. https://doi.org/10.1016/j.fertnstert.2016.02.005 [PubMed]
-
10.
Vaegter KK, Lakic TG, Olovsson M, Berglund L, Brodin T, Holte J. Which factors are most predictive for live birth after in vitro fertilization and intracytoplasmic sperm injection (IVF/ICSI) treatments? Analysis of 100 prospectively recorded variables in 8,400 IVF/ICSI single-embryo transfers. Fertil Steril. 2017; 107:641–48.e2. https://doi.org/10.1016/j.fertnstert.2016.12.005 [PubMed]
-
11.
van Loendersloot LL, van Wely M, Limpens J, Bossuyt PM, Repping S, van der Veen F. Predictive factors in in vitro fertilization (IVF): a systematic review and meta-analysis. Hum Reprod Update. 2010; 16:577–89. https://doi.org/10.1093/humupd/dmq015 [PubMed]
-
12.
Iliodromiti S, Kelsey TW, Wu O, Anderson RA, Nelson SM. The predictive accuracy of anti-Müllerian hormone for live birth after assisted conception: a systematic review and meta-analysis of the literature. Hum Reprod Update. 2014; 20:560–70. https://doi.org/10.1093/humupd/dmu003 [PubMed]
-
13.
Maseelall PB, Hernandez-Rey AE, Oh C, Maagdenberg T, McCulloh DH, McGovern PG. Antral follicle count is a significant predictor of livebirth in in vitro fertilization cycles. Fertil Steril. 2009; 91:1595–97. https://doi.org/10.1016/j.fertnstert.2008.11.001 [PubMed]
-
14.
Schisterman EF, Sjaarda LA, Clemons T, Carrell DT, Perkins NJ, Johnstone E, Lamb D, Chaney K, Van Voorhis BJ, Ryan G, Summers K, Hotaling J, Robins J, et al. Effect of Folic Acid and Zinc Supplementation in Men on Semen Quality and Live Birth Among Couples Undergoing Infertility Treatment: A Randomized Clinical Trial. JAMA. 2020; 323:35–48. https://doi.org/10.1001/jama.2019.18714 [PubMed]
-
15.
Calhaz-Jorge C, De Geyter C, Kupka MS, de Mouzon J, Erb K, Mocanu E, Motrenko T, Scaravelli G, Wyns C, Goossens V, Gliozheni O, Strohmer H, Obruca, et al, and European IVF-monitoring Consortium (EIM), and European Society of Human Reproduction and Embryology (ESHRE). Assisted reproductive technology in Europe, 2013: results generated from European registers by ESHRE. Hum Reprod. 2017; 32:1957–73. https://doi.org/10.1093/humrep/dex264 [PubMed]
-
16.
Wang YA, Healy D, Black D, Sullivan EA. Age-specific success rate for women undertaking their first assisted reproduction technology treatment using their own oocytes in Australia, 2002-2005. Hum Reprod. 2008; 23:1633–38. https://doi.org/10.1093/humrep/den135 [PubMed]
-
17.
Lintsen AM, Eijkemans MJ, Hunault CC, Bouwmans CA, Hakkaart L, Habbema JD, Braat DD. Predicting ongoing pregnancy chances after IVF and ICSI: a national prospective study. Hum Reprod. 2007; 22:2455–62. https://doi.org/10.1093/humrep/dem183 [PubMed]
-
18.
Bleil ME, Gregorich SE, Adler NE, Sternfeld B, Rosen MP, Cedars MI. Race/ethnic disparities in reproductive age: an examination of ovarian reserve estimates across four race/ethnic groups of healthy, regularly cycling women. Fertil Steril. 2014; 101:199–207. https://doi.org/10.1016/j.fertnstert.2013.09.015 [PubMed]
-
19.
Sabatini L, Zosmer A, Hennessy EM, Tozer A, Al-Shawaf T. Relevance of basal serum FSH to IVF outcome varies with patient age. Reprod Biomed Online. 2008; 17:10–19. https://doi.org/10.1016/s1472-6483(10)60287-8 [PubMed]
-
20.
Hsu A, Arny M, Knee AB, Bell C, Cook E, Novak AL, Grow DR. Antral follicle count in clinical practice: analyzing clinical relevance. Fertil Steril. 2011; 95:474–79. https://doi.org/10.1016/j.fertnstert.2010.03.023 [PubMed]
-
21.
Broer SL, Dólleman M, Opmeer BC, Fauser BC, Mol BW, Broekmans FJ. AMH and AFC as predictors of excessive response in controlled ovarian hyperstimulation: a meta-analysis. Hum Reprod Update. 2011; 17:46–54. https://doi.org/10.1093/humupd/dmq034 [PubMed]
-
22.
Majumder K, Gelbaya TA, Laing I, Nardo LG. The use of anti-Müllerian hormone and antral follicle count to predict the potential of oocytes and embryos. Eur J Obstet Gynecol Reprod Biol. 2010; 150:166–70. https://doi.org/10.1016/j.ejogrb.2010.02.029 [PubMed]
-
23.
Roberts SA, Hirst WM, Brison DR, Vail A, and towardSET collaboration. Embryo and uterine influences on IVF outcomes: an analysis of a UK multi-centre cohort. Hum Reprod. 2010; 25:2792–802. https://doi.org/10.1093/humrep/deq213 [PubMed]
-
24.
Li F, Ye T, Kong H, Li J, Hu L, Jin H, Su Y, Li G. Efficacies of different ovarian hyperstimulation protocols in poor ovarian responders classified by the POSEIDON criteria. Aging (Albany NY). 2020; 12:9354–64. https://doi.org/10.18632/aging.103210 [PubMed]
-
25.
Esteves SC, Roque M, Bedoschi GM, Conforti A, Humaidan P, Alviggi C. Defining Low Prognosis Patients Undergoing Assisted Reproductive Technology: POSEIDON Criteria-The Why. Front Endocrinol (Lausanne). 2018; 9:461. https://doi.org/10.3389/fendo.2018.00461 [PubMed]
-
26.
Polyzos NP, Drakopoulos P. Management Strategies for POSEIDON’s Group 1. Front Endocrinol (Lausanne). 2019; 10:679. https://doi.org/10.3389/fendo.2019.00679 [PubMed]
-
27.
Leijdekkers JA, Torrance HL, Broekmans FJ. Reply: The low responder according to the POSEIDON criteria: is the prognosis really poor? Hum Reprod. 2019; 34:2557–58. https://doi.org/10.1093/humrep/dez195 [PubMed]
-
28.
Wang R, Lin S, Wang Y, Qian W, Zhou L. Comparisons of GnRH antagonist protocol versus GnRH agonist long protocol in patients with normal ovarian reserve: A systematic review and meta-analysis. PLoS One. 2017; 12:e0175985. https://doi.org/10.1371/journal.pone.0175985 [PubMed]
-
29.
Toftager M, Sylvest R, Schmidt L, Bogstad J, Løssl K, Prætorius L, Zedeler A, Bryndorf T, Pinborg A. Quality of life and psychosocial and physical well-being among 1,023 women during their first assisted reproductive technology treatment: secondary outcome to a randomized controlled trial comparing gonadotropin-releasing hormone (GnRH) antagonist and GnRH agonist protocols. Fertil Steril. 2018; 109:154–64. https://doi.org/10.1016/j.fertnstert.2017.09.020 [PubMed]